Venous Insufficiency Explained – What It Is and How to Deal With It
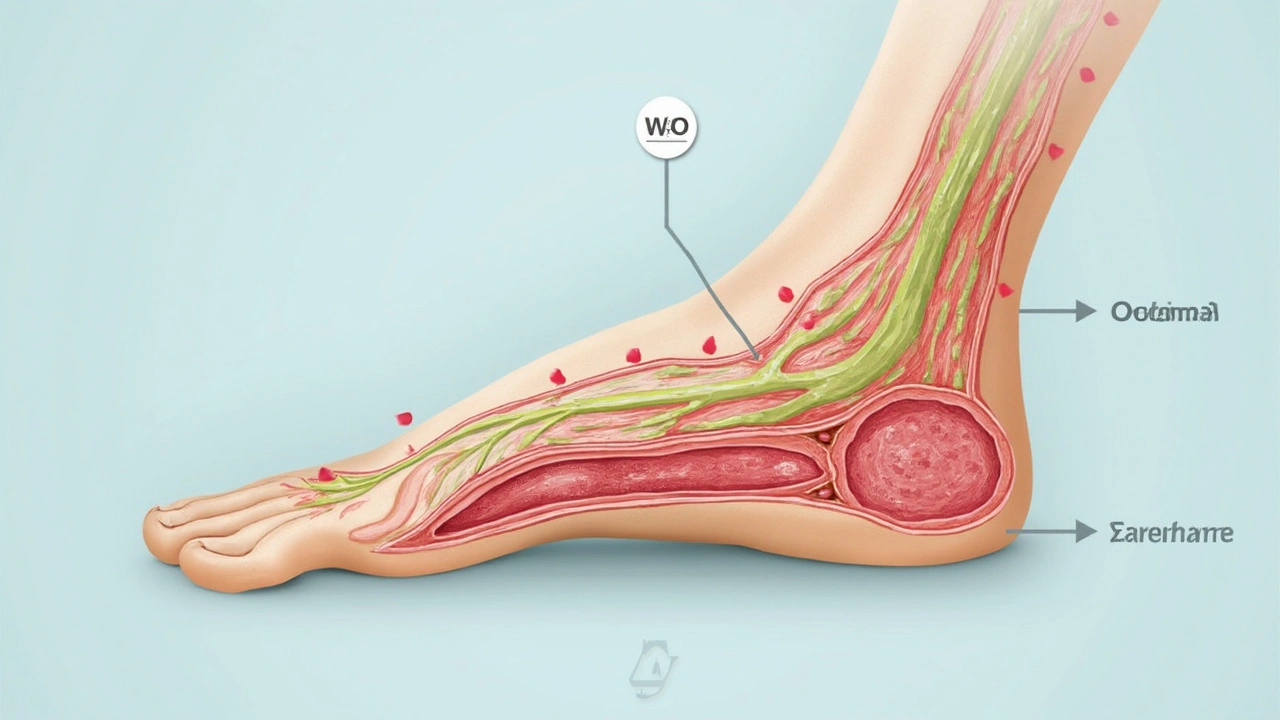
If you’ve ever noticed aching calves, swollen ankles, or dark veins crawling up your legs, you might be looking at venous insufficiency. It’s basically a weak valve problem in your veins that stops blood from flowing back up to your heart. Instead, blood pools in the lower legs, causing the uncomfortable symptoms you’ve probably felt.
What Triggers Venous Insufficiency?
Several everyday factors can knock your vein valves off balance. Standing or sitting for long periods—think office jobs or long flights—puts constant pressure on leg veins. Genetics also play a big role; if your parents had varicose veins, chances are yours might follow suit. Being overweight adds extra load, while pregnancy stretches the veins and raises pressure inside the abdomen. Even age matters, as veins lose elasticity over time, making it harder for the valves to close tightly.
Other culprits include smoking (which damages blood vessels), a sedentary lifestyle, and injuries that scar or compress veins. If you’ve had a deep‑vein thrombosis (DVT) in the past, the damage left behind can also lead to chronic venous insufficiency later on.
How to Manage and Feel Better
The good news? You don’t need surgery to get relief. Simple lifestyle tweaks can cut swelling and pain dramatically. First, move the blood. Take a short walk every hour, wobble your calves while sitting, or do ankle pumps—flexing your foot up and down—to push blood upward.
Compression stockings are another powerhouse. They apply gentle pressure, helping veins squeeze blood back toward the heart. Start with a light‑to‑moderate compression level; you can step up if symptoms persist. Make sure the stockings fit snugly but aren’t cutting off circulation.
Weight management matters too. Shedding even a few pounds reduces pressure on the leg veins, easing swelling. Pair a balanced diet with regular activity, and you’ll notice the difference in how your legs feel after a day on your feet.
Elevate your legs whenever you can. Prop them up on a pillow at night or while watching TV. Aim for the heart level or slightly higher to encourage draining. If you’re prone to night cramps, a warm foot soak before bed can improve circulation.
When over‑the‑counter isn’t enough, talk to a doctor about prescription options. Medications that strengthen vein walls or improve blood flow—like micronized purified flavonoid fractions (MPFF)—can be helpful. In severe cases, a vein specialist might suggest minimally invasive procedures such as endovenous laser therapy or sclerotherapy.
Lastly, keep an eye on skin changes. Persistent redness, itching, or ulcer formation needs prompt medical attention. Early treatment can prevent infections and more serious complications.
Venous insufficiency is a common, manageable condition. By staying active, using compression, watching your weight, and seeking professional advice when needed, you can keep your legs comfortable and healthy.
-
24
When fluids accumulate in body tissues, it leads to oedema, a condition that can cause swelling and discomfort. Venous insufficiency, a common cause, occurs when veins struggle to send blood from the limbs back to the heart. This article explores why this happens, what symptoms to watch for, and how it can be managed. We'll delve into practical tips and treatment options that might ease the burden of this common issue.
Categories
Tags Weight
- online pharmacy
- side effects
- dietary supplement
- medication safety
- dosage
- online pharmacy safety
- drug interactions
- health benefits
- allergy relief
- autoimmune disease
- antibiotic
- pharmacy reviews
- affordable antidepressant
- gut health
- safe online meds
- prevention
- patient safety
- NSAIDs
- drug interaction
- blood thinners