Swelling in the body can be more than a temporary nuisance—it’s a signal that something isn't quite right. That's where oedema comes into play. Essentially, it's when your body tissues cling onto excess fluids, making you puffier than your morning coffee alone can explain. Now, not everyone with puffiness has a medical issue, but when it comes to oedema, paying attention to your body pays off.
Often, venous insufficiency is a silent partner in crime here. This happens when your veins are having a hard time sending blood from your legs back up to your heart. While it sounds technical, it’s actually more common than you might think. In cases of venous insufficiency, you're left with those tired aching legs, and maybe even swelling that doesn't seem to quit.
- Understanding Oedema: What Is It?
- Venous Insufficiency Explained: The Basics
- Common Causes and Symptoms
- Effective Treatments and Management
- Practical Tips for Everyday Life
Understanding Oedema: What Is It?
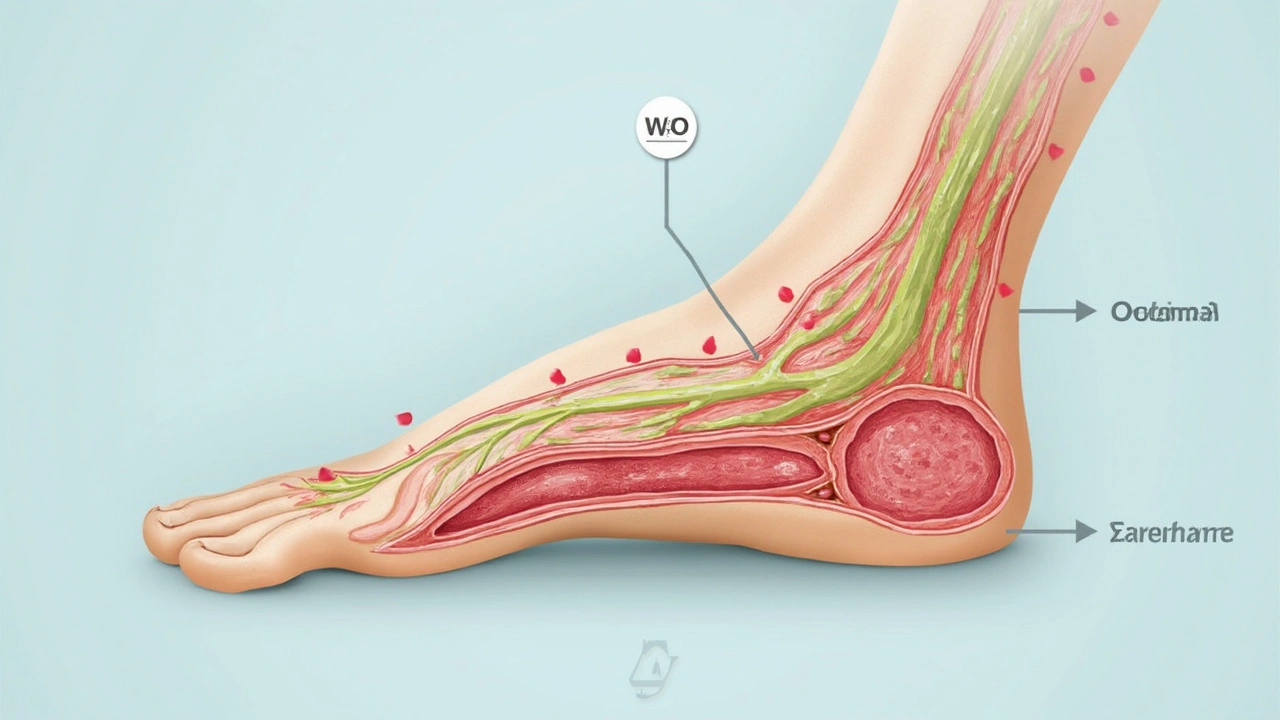
So, what is oedema exactly? In simple terms, it's swelling caused by fluid retention. Your body holds onto fluids it normally wouldn't, which builds up in the spaces between your cells. This buildup often affects your hands, feet, ankles, and legs—but it can appear anywhere.
Oedema is often easy to spot: you might notice your skin looks a bit stretched or shiny. Press gently on the swollen area, and if it leaves an indent, you’ve probably got oedema. Doctors sometimes call this the 'pitting' effect, and it's a dead giveaway.
Different Types of Oedema
Oedema isn’t just one-size-fits-all. There are several types:
- Peripheral Oedema: This is the kind most people experience, affecting limbs.
- Pulmonary Oedema: It’s a serious one, as fluid collects in the lungs, making breathing tough.
- Macular Oedema: Fluid builds up in the eyes, impacting vision.
- Cerebral Oedema: Occurs in the brain and can be quite severe.
Your body’s lymphatic system plays a big role here, too. It usually helps manage fluid balance. If it's out of whack, oedema can occur. Combined with issues like venous insufficiency, you're more likely to spot the signs.
The Science Behind It
Let's talk circulation for a moment. Picture it: your blood is a constant flow, delivering nutrients while removing waste products. If that flow stalls, pressure builds, and fluids seep out of blood vessels into tissues. That's how swelling starts.
Aside from the obvious puffiness, the causes behind oedema can vary. It could be as benign as sitting too long on an airplane or as serious as heart failure. Keep those eyes peeled for symptoms that won't go away.
Venous Insufficiency Explained: The Basics
So, what exactly is this venous insufficiency thing? At its core, it's when the veins in your legs struggle to pump blood back to your heart. Imagine a river flowing uphill—it's gonna hit some snags, right? Veins have little valves that should keep the blood moving upward, but when they don’t close properly, blood can leak back down and pool in the legs, which isn’t what you want.
What Causes It?
Several factors might steer you onto the path of venous insufficiency. Age can be a factor, as vein walls and valves can get weaker over time. If you're pregnant, that extra pressure can mess with vein performance too. Also, family history plays a role. If your folks had it, you might too.
Signs to Watch For
Keep an eye out for tired, heavy legs that just don’t get better with rest. That’s one of the big clues. Swelling, usually around the ankles, is often one of the first signs. It might ease after a night of rest, but if it sticks around, take note. Then there’s the skin—it might change color or texture, getting thin and itchy.
Why It Matters
Ignoring venous insufficiency isn’t the best game plan. Over time, those pesky symptoms can worsen if you don't manage them. In severe cases, you could face ulcers or open sores, particularly around the ankles, and believe me, you don't want that.
The Stats
Here's a little reality check—a bunch of folks deal with this. Studies show that around 25% of adults experience some form of venous disorder. That’s a lot, right? So, if it happens to you, know you’re not alone in this.

Common Causes and Symptoms
Let's face it—our bodies don't always give us a straight answer when something's up. So, when it comes to understanding what's behind oedema, a few usual suspects come to mind.
What Causes Oedema?
First on the list is venous insufficiency, where your veins are not up for the job of pushing blood back to the heart efficiently. Gravity's no help here, either. Then there are things like sitting too long on a plane (hello, economy class syndrome!), or even standing on your feet all day.
Long-term conditions can also play their part. Conditions like heart failure or kidney disease make your body retain more fluids, which leads to—yep, you guessed it—swelling. Hormonal changes, especially during pregnancy, and some medications like steroids or blood pressure drugs can tip the scale toward unnecessary fluid retention.
Spotting the Symptoms
Symptoms can vary, but here’s what’s generally on the list. If you notice swelling that's not just in your feet but climbs up into your legs, it's a sign. Pressed spots that leave a dimple, known as pitting, is another clue. And if your shoes feel like a vice around your feet when they used to fit like a dream, take note.
- A heavy, achy feeling especially in the legs.
- Swelling that gets worse as the day goes on.
- Tightness or puffiness of the skin, especially after meals or in the evenings.
Sometimes, numbers help paint the picture. Did you know that chronic venous insufficiency affects nearly 20% of adults? That's quite a chunk of us, and it's why noticing these signs matters.
Effective Treatments and Management
So, you know about oedema and venous insufficiency, and you're wondering how to manage it effectively. Fortunately, there are plenty of strategies to help keep the swelling at bay. It starts with simple lifestyle tweaks and goes up to medical interventions depending on the severity of the issue.
Getting Moving: The Power of Exercise
Yeah, it’s the age-old advice to get moving, but it really helps. Regular exercise improves blood circulation, making your veins more efficient at returning blood to the heart. Even something as simple as walking can put those veins to work. Aim for at least 30 minutes of light exercise daily to see a noticeable difference.
Elevate and Compress: A Simple Fix
Feeling swollen after a long day? Elevate your legs above heart level for a bit. It’s an easy way to encourage fluid drainage. Look into compression stockings, too. These nifty socks apply pressure to your lower legs and aid in reducing swelling and improving circulation.
Watch What You Eat
Keeping an eye on your diet can make a big difference. Reducing salt intake can help as salt can cause your body to hold on to fluids. Opt for more fruits and veggies, and drink plenty of water to stay hydrated.
Medical Options
When home remedies and lifestyle changes aren't cutting it, it's time to talk to a doc. They might suggest medications like diuretics that help reduce excess fluid from the body. In some cases, procedures intended to improve vein function might be necessary. Always consult with a healthcare professional to explore these alternatives.
Stay Informed
Tracking your symptoms and understanding triggers can be immensely helpful. Educating yourself about the conditions not only empowers you but also helps you make informed decisions. Consider keeping a journal of your symptoms, which might give insights into patterns that you can discuss with a doctor.

Practical Tips for Everyday Life
Managing oedema and venous insufficiency doesn't have to be overwhelming. There are simple adjustments you can make to your routine that can make a significant difference. Let's explore some ways you can ease symptoms and get on with living your life comfortably.
Stay Active
Movement is magic when it comes to improving circulation and reducing fluid retention. Try incorporating more physical activity into your day—walking, swimming, or cycling can all help. Just aim for at least 30 minutes a day, and you’ll likely notice those puffy ankles behaving better.
Keep Propped Up
Gravity can be both a friend and a foe. Elevating your legs above heart level for about 15 minutes several times a day can encourage blood flow and decrease swelling.
Watch Your Diet
Certain tweaks to what you eat might help too. Reduce salt intake, drink plenty of water, and include foods like bananas and avocados that are high in potassium, as this can help balance things out.
Consider Compression
Compression stockings? Yes, they may not be the most glamorous, but these snug socks can work wonders by helping prevent fluid retainment in your legs. Just make sure you have the right fit, or they won't be as effective.
Stay Cool
In hotter weather, oedema can worsen, so keeping cool is beneficial. Air conditioning, cool showers, or a simple splash of water on your feet can offer relief.
- Take regular breaks if you’re standing or sitting for long periods.
- Contact a healthcare provider if symptoms persist or worsen.
Remember, these steps aren't one-size-fits-all solutions, but they offer a solid start to managing oedema and venous insufficiency day-to-day.

Kathy Butterfield
July 18, 2025 AT 16:18Hey everyone! 👋 I really appreciate this post shedding light on oedema and venous insufficiency because not many people understand how serious and uncomfortable these conditions can get.
From my experience, managing swelling can be quite tricky especially when it's caused by veins not pumping blood efficiently. It’s super helpful that the article talks about symptoms because sometimes we just think "oh it's normal swelling" but it might be something more.
Also, practical tips—do those usually involve compression stockings or lifestyle changes? I’ve been curious about what really works long-term.
Anyone here been through treatments or maybe natural remedies that helped? I’m always looking for some good advice! 😊
Thanks for bringing this up!
Richard Wieland
July 18, 2025 AT 17:08This is quite a lucid introduction to the complications that come with venous insufficiency, honestly.
It’s fascinating how something as simple as blood flow inefficiency can cause such a cascade of discomfort and medical issues. The article explains things clearly, which is vital because understanding the problem fully helps in not ignoring symptoms.
Does anyone here know if the causes differ significantly based on age or lifestyle? I assume it’s not just genetics but habits also play a role.
Having a systematic approach to treatment and prevention would certainly ease the burden folks face daily.
Deborah Escobedo
July 18, 2025 AT 19:05Thanks for this informative piece. The connection between oedema and venous insufficiency is often overlooked.
From my clinical experience, early detection makes a huge difference in outcomes for patients dealing with these.
Managing such conditions revolves around lifestyle adaptations and proper medical support. Compression therapy is quite effective as well. However, it’s important people take symptoms seriously and seek advice before it becomes severe.
I hope readers feel encouraged to consult their healthcare providers if they notice swelling that won’t go away.
Dipankar Kumar Mitra
July 18, 2025 AT 19:55Seriously, why do people ignore these signs until it turns into full-blown misery? Venous insufficiency isn't just about some mild swelling; it’s a sneaky condition that can wreck your quality of life.
We all should be more aware and proactive. Compression stockings? Yeah, they work but only if you are consistent and not lazy about it.
And let's not even get started on the nonsense advice from people trying out ‘miracle cures’. Stick to what science says people.
Anyone else tired of myths surrounding this?
Tracy Daniels
July 18, 2025 AT 23:48Hey, I just wanted to add a bit about emotional support for folks dealing with these issues. Sometimes the discomfort and visible swelling can make people self-conscious or anxious.
Knowing that there are community and professional resources to help manage both physical and mental health is vital. 😊
Also, regular check-ins with your doctor to monitor symptoms can really make a difference in preventing complications.
Let’s keep talking about these less discussed conditions and support each other!
Hoyt Dawes
July 19, 2025 AT 03:25Honestly, I’m skeptical about a ton of these suggested treatments. Compression stockings and the like just seem to be band-aid solutions to me.
If the veins are weak, shouldn’t we be looking at more permanent fixes or even questioning why our healthcare system doesn’t push harder for them?
Not that anyone ever wants to hear this from a drama king, but it feels like a lot of hype around symptoms and not enough about tackling root causes.
Am I alone in feeling this way?
Jeff Ceo
July 19, 2025 AT 06:12Let's cut the fluff. These conditions can get serious fast if you're not vigilant. Compression stockings, lifestyle changes, and medical supervision are non-negotiable for anyone diagnosed with this.
People waiting too long make things worse and then cry foul when treatments get complicated and expensive.
Better to be aggressive at managing symptoms early rather than passive and suffer later. Period.
David Bui
July 19, 2025 AT 07:02First off, the explanation could use a bit more clarity. There’s no excuse for sloppy punctuation in an informative post like this.
Moreover, the symptoms list could be expanded. Many don’t realize the range of effects venous insufficiency can have, including skin changes and ulcers.
For those interested, a detailed breakdown of venous anatomy and physiology would help grasp why these veins fail to return blood properly.
Let’s get facts straight with precision, folks.
Alex V
July 19, 2025 AT 07:52Typical health content, glossing over the real reasons why these problems have exploded recently. It's not just biology, folks.
Big pharma wouldn’t want you to know that lifestyle, diet, and even industrial food processing are part of the real cause behind the 'common' venous insufficiency epidemic.
Take a minute to research the hidden truths, and don’t buy into the surface explanations only.
Meanwhile, yeah compression socks are useful, but they’re just treating symptoms, not the cause!
Robert Jackson
July 19, 2025 AT 10:38Right, less conspiracy and more facts please.
I find it annoying when people jump to such extremes without acknowledging common medical consensus.
The condition has clear pathophysiological mechanisms well documented for decades, no need to invent hidden agendas.
Focus on evidence-based treatment and stop muddying the waters.
Maricia Harris
July 19, 2025 AT 12:35Honestly, some folks here are just drama queens, blowing things way out of proportion.
This condition is common and manageable. No need for all the panic or conspiracy theories.
Like, get a grip and listen to your doctors, wear your stockings, and chill.
Trust me, it’s far from the apocalypse some here paint it to be.