Autoimmune Disease: What You Need to Know
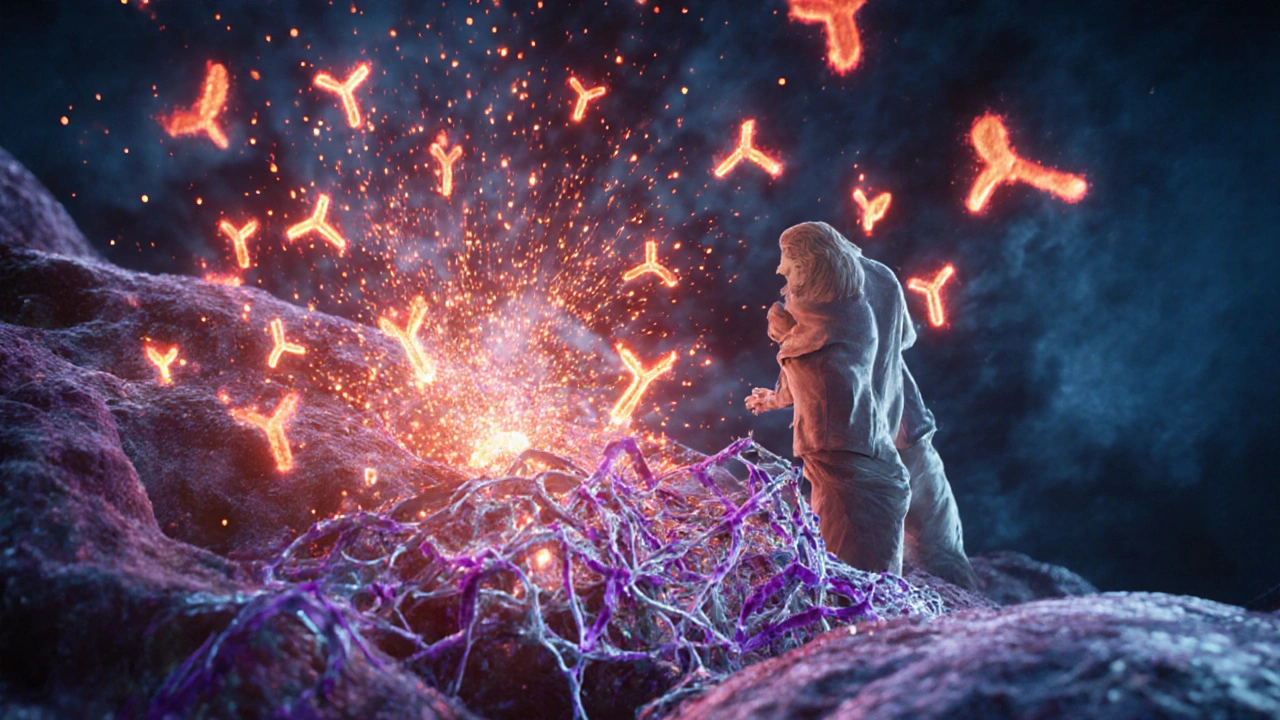
Ever wonder why your body sometimes attacks itself? That’s the core idea behind an autoimmune disease. Your immune system, which is supposed to protect you, gets confused and starts targeting healthy tissue. This can cause pain, fatigue, and a host of other symptoms that vary a lot depending on the condition.
People often think autoimmune problems are rare, but they affect millions worldwide. The good news is that doctors now have many tools to diagnose early and manage the disease, so you can keep living a normal life.
Common Autoimmune Conditions
There are more than 80 known autoimmune diseases. Here are a few you’ll hear about most often:
- Rheumatoid arthritis – joints become swollen, painful, and stiff.
- Hashimoto’s thyroiditis – the thyroid gets attacked, leading to low hormone levels.
- Multiple sclerosis (MS) – the nervous system’s protective coating is damaged, causing vision problems and muscle weakness.
- Systemic lupus erythematosus (Lupus) – a wide‑range disease that can hit skin, kidneys, joints, and more.
- Psoriasis – skin cells grow too fast, creating red, scaly patches.
Each condition has its own set of warning signs, but fatigue, unexplained weight changes, and lingering pain are common threads. If you notice a pattern that doesn’t fit a simple infection or injury, it’s worth asking a doctor to check for an autoimmune trigger.
Managing Symptoms and Treatment
There’s no one‑size‑fits‑all cure, but many strategies help keep symptoms in check. Medication is often the first line of defense. Doctors may prescribe:
- Non‑steroidal anti‑inflammatory drugs (NSAIDs) for pain and swelling.
- Corticosteroids like prednisolone (found in products such as Pred Forte eye drops) to calm intense inflammation.
- Disease‑modifying antirheumatic drugs (DMARDs) to slow the disease’s progress.
- Biologics that target specific parts of the immune response.
Alongside meds, lifestyle tweaks make a big difference. Regular gentle exercise improves joint flexibility and reduces fatigue. A balanced diet rich in omega‑3 fatty acids, antioxidants, and low‑glycemic foods can lower inflammation. Stress management is crucial—stress hormones can flare up autoimmune activity, so techniques like deep breathing, yoga, or short daily walks help.
Our tag page also gathers articles that touch on related topics, such as how stress can trigger movement disorders (see the “Stress and Dyskinesia” post) or how certain eye drops are used for autoimmune‑related eye inflammation (check the “Pred Forte” guide). These pieces give you deeper insight into how specific treatments fit into the broader autoimmune picture.
Finally, stay informed. New research on biologics, personalized medicine, and gut‑immune connections is emerging fast. Subscribing to reliable health news sites, joining patient support groups, and speaking openly with your healthcare team keep you ahead of changes that could improve your quality of life.
Autoimmune disease may feel overwhelming at first, but with the right knowledge and a proactive plan, you can manage it effectively. Keep asking questions, track how you feel, and remember that many people live full lives while navigating these conditions.
-
2
Explore how the immune system malfunctions in lupus, the key players involved, triggers, treatments, and lifestyle steps to keep flares under control.
-
8
Diet is a game-changer for people with rheumatoid arthritis, helping to manage inflammation and ease symptoms. This article explores what science really says about food choices, from anti-inflammatory diet tips to the surprising impact of certain meal patterns. Dive into the foods that can ease daily pain—and those that can make it worse. Easy tweaks at the grocery store may help you take control. Real facts, clear advice, and plenty of practical examples make managing rheumatoid arthritis possible, one meal at a time.
Tags Weight
- online pharmacy
- side effects
- medication safety
- dietary supplement
- dosage
- online pharmacy safety
- drug interaction
- drug interactions
- generic medications
- generic drugs
- health benefits
- allergy relief
- autoimmune disease
- antibiotic
- pharmacy reviews
- affordable antidepressant
- gut health
- safe online meds
- prevention
- patient safety