Lupus Immune System Explorer
Explore how different immune components contribute to lupus and how treatments can help manage the condition.
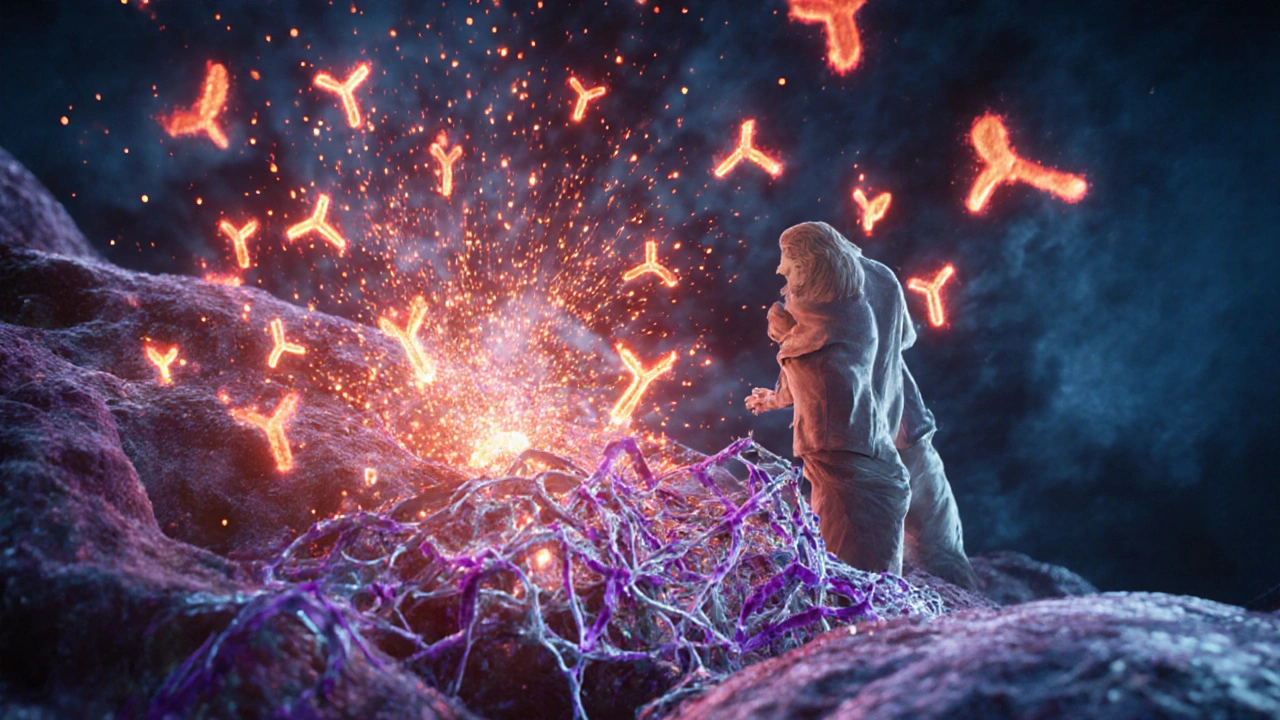
B Cells
Produce autoantibodies that target the body's own proteins. In lupus, they become hyperactive and create harmful immune complexes.
T Cells
Regulatory and helper cells that coordinate immune responses. In lupus, they lose their ability to control B cell activity.
Cytokines
Signaling proteins that amplify inflammation. Excessive cytokine production leads to a "cytokine storm" causing organ damage.
Autoantibodies
Antibodies that target self-antigens like DNA and proteins. They form immune complexes that deposit in tissues and cause inflammation.
Skin
Butterfly rash, photosensitivity, skin lesions due to autoantibody-driven inflammation.
Joints
Painful swelling resembling arthritis caused by cytokine-mediated synovial inflammation.
Kidneys
Lupus nephritis from immune complex deposits in glomeruli leading to kidney failure.
UV Radiation
Sun exposure can trigger skin flares and systemic disease activity.
Infections
Viruses like EBV can prime autoreactive T cells through molecular mimicry.
Smoking
Promotes oxidative stress that worsens B-cell auto-reactivity.
Treatment Approach
Current therapies aim to reset the immune balance without compromising overall immunity. Common treatments include:
- NSAIDs: For pain relief in joints and muscles
- Corticosteroids: Rapid suppression of cytokine production during flares
- Antimalarials: Modulate T-cell activation and reduce flare frequency
- Immunosuppressants: Inhibit B-cell proliferation for severe cases
- Biologics: Targeted agents like belimumab or anifrolumab
Lifestyle Support
Supporting immune balance through lifestyle changes can help reduce flares:
- Sun Protection: Use SPF 30+ sunscreen and protective clothing
- Quit Smoking: Reduces oxidative stress
- Balanced Diet: Rich in omega-3s, antioxidants, and vitamin D
- Stress Management: Practice yoga or meditation
- Exercise: Low-impact activities to maintain health
Quick Takeaways
- Lupus is an autoimmune disease where the lupus immune system attacks healthy tissue.
- Faulty B cells, T cells, and cytokine storms fuel the inflammation.
- Genetic factors and environmental triggers tip the balance toward disease.
- Treatments aim to calm the immune system without wiping it out.
- Lifestyle tweaks can support immune balance and reduce flare‑ups.
When doctors talk about lupus, they’re really talking about a runaway immune response. Understanding why the immune system goes haywire helps patients and caregivers make sense of symptoms, choose therapies, and adopt habits that keep flares at bay.
What Is Lupus and Why Does the Immune System Matter?
Lupus is a chronic autoimmune disease that can affect skin, joints, kidneys, brain, and many other organs. The most common form, Systemic Lupus Erythematosus (SLE), is notorious for its unpredictable flare‑ups.
In a healthy body, the Immune System a network of cells, proteins, and signaling pathways that defends against infections distinguishes self from non‑self. Lupus flips that script-immune cells start seeing the body’s own proteins as invaders.
Core Immune Players Gone Awry
The immune mess in lupus can be broken down into a few key actors:
- B cells white blood cells that produce antibodies become hyper‑active, churning out autoantibodies that bind to self‑antigens.
- T cells regulatory and helper cells that coordinate immune responses lose their ability to keep B cells in check.
- Cytokines signaling proteins that amplify inflammation soar, creating a cytokine storm that damages organs.
- Autoantibodies antibodies targeting the body’s own DNA, proteins, and phospholipids form immune complexes that lodge in tissues.
The combined effect is a self‑sustaining loop: autoantibodies trigger complement activation, which releases more cytokines, which further stimulates B and T cells. Breaking any link in that chain can halt a flare.
Why Do Some People Get Lupus? Genetics and the Environment
Not everyone with a faulty immune system develops lupus. Two broad categories of risk factors stack up:
| Factor | Type | Typical Influence |
|---|---|---|
| HLA‑DR2/DR3 | Genetic predisposition | Increases likelihood of autoantibody production by 2‑3× |
| Complement deficiency (C1q, C4) | Genetic | Impairs clearance of immune complexes, raising organ damage risk |
| UV radiation | Environmental | Triggers skin lesions and can ignite systemic flares |
| Smoking | Environmental | Promotes oxidative stress, worsening B‑cell auto‑reactivity |
| Infections (EBV, CMV) | Environmental | Provide molecular mimicry that can prime autoreactive T cells |
Researchers estimate that over 70% of lupus patients carry at least one high‑risk gene, but a triggering event-like a sunburn or a viral infection-often lights the fuse.

From Immune Chaos to Clinical Symptoms
Different organ systems feel the impact of immune mis‑recognition in unique ways:
- Skin: Autoantibody‑driven inflammation leads to the classic “butterfly rash” on the cheeks.
- Joints: Cytokine‑mediated synovial swelling causes pain that mimics arthritis.
- Kidneys: Immune complexes deposit in glomeruli, sparking lupus nephritis, the leading cause of renal failure in young adults.
- Brain: Neuro‑inflammation from cytokines can produce headaches, mood swings, or seizures.
- Blood: Auto‑immune hemolysis and thrombocytopenia arise when antibodies attack red cells and platelets.
Because the same immune mechanisms can affect many organs, lupus is called “the great imitator.” That’s why doctors rely on a combination of blood tests (ANA, anti‑dsDNA, complement levels) and clinical clues to confirm a diagnosis.
Targeting the Immune System: Current Treatments
Therapies for lupus aim to reset the immune balance without leaving patients defenseless against infections. The main categories are:
- Non‑steroidal anti‑inflammatory drugs (NSAIDs): Provide pain relief for joint and muscle aches.
- Corticosteroids: Rapidly suppress cytokine production; used for acute flares but tapered to avoid long‑term side effects.
- Antimalarials (hydroxychloroquine): Modulate T‑cell activation and have been shown to lower flare frequency by up to 50%.
- Immunosuppressants (azathioprine, mycophenolate, cyclophosphamide): Inhibit B‑cell proliferation, essential for severe kidney or CNS involvement.
- Biologics: Targeted agents like belimumab (anti‑BLyS) reduce B‑cell survival; recent trials with anifrolumab (anti‑typeI interferon receptor) show promise for skin and joint symptoms.
Choosing the right mix depends on which organs are active, the patient’s age, pregnancy plans, and tolerance for side effects. Regular labs help tweak doses before toxicity sneaks up.
Everyday Ways to Support a Balanced Immune Response
Medical treatment is the backbone, but lifestyle tweaks can tip the immune system toward calm:
- Sun protection: Broad‑spectrum SPF30+ sunscreen and protective clothing cut UV‑triggered skin flares.
- Quit smoking: Eliminates a major source of oxidative stress that fuels B‑cell auto‑reactivity.
- Balanced diet: Omega‑3 rich fish, antioxidants (berries, leafy greens), and adequate vitaminD have been linked to lower disease activity scores.
- Stress management: Mind‑body practices (yoga, meditation) lower cortisol, which otherwise skews cytokine release.
- Regular exercise: Low‑impact activities improve cardiovascular health without over‑activating the immune system.
Patients should keep a symptom diary. Patterns often emerge-like a flare a week after a stressful deadline-making it easier to adjust triggers.
Future Directions: Precision Medicine for Lupus
Scientists are zeroing in on the exact immune pathways that differ between patients. Emerging tools include:
- Gene‑expression panels: Identify patients with high interferon‑signature scores who may respond best to anifrolumab.
- Single‑cell sequencing: Maps rogue B‑cell clones, paving the way for personalized B‑cell depletion strategies.
- Autoantibody profiling: Distinguishes sub‑types of lupus that preferentially affect the kidneys versus the skin.
These advances promise a future where therapy is matched to a patient’s immune fingerprint, reducing trial‑and‑error prescribing.
Frequently Asked Questions
Can diet really affect lupus activity?
Yes. A diet rich in omega‑3 fatty acids, antioxidants, and adequate vitaminD can dampen inflammation. Conversely, excess saturated fat and processed sugars may boost cytokine production, worsening flares.
Why do some lupus patients have normal antibody tests?
Early‑stage disease or organ‑specific involvement (like isolated skin lesions) may not yet produce high‑titer autoantibodies. Clinical judgment and repeat testing are essential.
Is it safe to get vaccinated while on immunosuppressants?
Inactivated vaccines (flu, COVID‑19, pneumococcal) are generally safe and recommended. Live vaccines should be avoided or timed carefully with your rheumatologist.
What causes kidney damage in lupus?
Immune complexes settle in the kidney’s filtering units, activating complement and recruiting inflammatory cells. This leads to scarring and reduced filtration if untreated.
How long does it take for a new medication to work?
Most immunosuppressants show measurable improvement within 4-8weeks, while biologics may need up to 12weeks to reach full effect. Monitoring labs helps gauge response.

Matthew Tedder
October 2, 2025 AT 12:27Adding a daily routine of gentle movement and stress‑relief practices can really help keep the immune system from overreacting. Even a short walk or a few minutes of deep breathing each day makes a difference. I always remind folks that consistency beats intensity when it comes to lifestyle tweaks.
Cynthia Sanford
October 3, 2025 AT 19:00Totally love how the post breaks down the B‑cell drama – it makes sense why we need hydroxychloroquine to keep those auto‑antibodies in check. The diet tips are on point, especially the omega‑3 suggestion. Keep sharing this kind of info, it definitly helps the community!
Karen McCormack
October 5, 2025 AT 01:34One could argue that the immune system is a fickle philosopher, constantly questioning self versus other. In lupus, that existential crisis turns pathological, spawning auto‑antibodies that betray the host. The interplay of genetics and environment reads like a tragic poem, each stanza a trigger. Yet, within that chaos, targeted biologics offer a hopeful stanza of redemption. It's a reminder that even the most errant mind can be guided back to balance.
Earl Hutchins
October 6, 2025 AT 08:07The immune cascade in lupus can be visualized as a series of dominoes. First, genetic predisposition tips the first piece. Then an environmental nudge such as UV exposure or an infection pushes the next. B‑cells respond by producing auto‑antibodies that form immune complexes. Those complexes settle in tissues and ignite complement activation. Complement fragments attract more inflammatory cells. Cytokines surge and create a feedback loop that fuels further B‑cell activation. T‑reg cells lose their suppressive grip, allowing helper T‑cells to amplify the response. The resulting cytokine storm damages organs like skin, joints, and kidneys. Clinically this shows up as rash, arthritis, and nephritis. Early intervention with NSAIDs can blunt the pain but does not halt the underlying loop. Corticosteroids act quickly to dampen cytokine production and buy time. Antimalarials such as hydroxychloroquine modulate T‑cell signaling and lower flare frequency. For severe organ involvement, immunosuppressants like mycophenolate target proliferating B‑cells. Biologics such as belimumab specifically neutralize BAFF, reducing B‑cell survival. Finally, lifestyle measures-sun protection, smoking cessation, balanced diet-address the external triggers that keep the dominoes falling. Together, these strategies aim to break the chain and restore equilibrium.
Tony Bayard
October 7, 2025 AT 14:40When you look at the trigger list, UV light often feels like the sneaky antagonist, lighting up skin cells and provoking auto‑antibody attacks. Infectious agents such as EBV can masquerade as self‑proteins, confusing T‑cells. Smoking isn’t just a habit; it delivers oxidative stress that primes B‑cells to misbehave. Stress hormones also tip the cytokine balance toward inflammation. Recognizing these cues early lets patients adjust habits before a full‑blown flare erupts.
Oliver Bishop
October 8, 2025 AT 21:14American research is leading the way in lupus breakthroughs!
johnson mose
October 10, 2025 AT 03:47I've seen patients swear by keeping a flare diary. When you chart UV exposure, stress levels, and diet, patterns start to emerge. It’s almost cinematic watching the “cause and effect” play out over weeks. That data can guide both medication adjustments and lifestyle tweaks. Sometimes the smallest change, like swapping coffee for tea, makes a noticeable difference.
Charmaine De Castro
October 11, 2025 AT 10:20That’s a solid observation. Documenting triggers empowers patients to take control and work with their doctors more effectively.
shashi Shekhar
October 12, 2025 AT 16:54Sure, let’s all trust the pharmaceutical giants who have never hidden side effects. Meanwhile, the “natural cure” crowd will just keep posting memes about vitamin D. Nothing like a good old conspiracy to spice up a medical discussion.
Marcia Bailey
October 13, 2025 AT 23:27Everyone’s perspective matters, and sharing evidence‑based tips helps us all stay informed 😊. Let’s keep the conversation respectful and focused on what truly helps patients.