Warfarin to DOAC Switch Calculator
INR-Based Switch Timing Calculator
Enter your most recent INR value to determine safe switching time to a DOAC.
Switching from warfarin to a direct oral anticoagulant (DOAC) isn’t just a change in pill color-it’s a shift in how your body manages blood clotting. For many people, this switch means fewer blood tests, less dietary worry, and a lower risk of dangerous bleeding. But if done wrong, it can lead to strokes, clots, or serious bleeding. The key isn’t just choosing a DOAC-it’s doing it right, at the right time, with the right patient in mind.
Why Switch from Warfarin?
Warfarin has been the go-to blood thinner for over 70 years. But it’s finicky. You need regular INR blood tests-sometimes every week-to make sure your dose is on target. Too low, and you risk a clot. Too high, and you could bleed internally. You also have to watch what you eat. Leafy greens, cranberry juice, even some antibiotics can throw your INR off balance. DOACs like dabigatran, rivaroxaban, apixaban, and edoxaban don’t need those weekly blood tests. They work more predictably. Your kidney function matters, but you don’t need to check INR every time you take a dose. That’s why, especially after the pandemic, doctors started pushing this switch. Fewer clinic visits, less stress, fewer interactions.When Is It Safe to Switch?
Not everyone can switch. And not everyone should. The biggest red flag? Prosthetic mechanical heart valves. DOACs are not approved for these patients. Warfarin is still the only option here. Other reasons to avoid switching:- Severe kidney disease (CrCl under 15-30 mL/min, depending on the DOAC)
- Advanced liver disease (Child-Pugh Class C)
- Pregnancy or breastfeeding
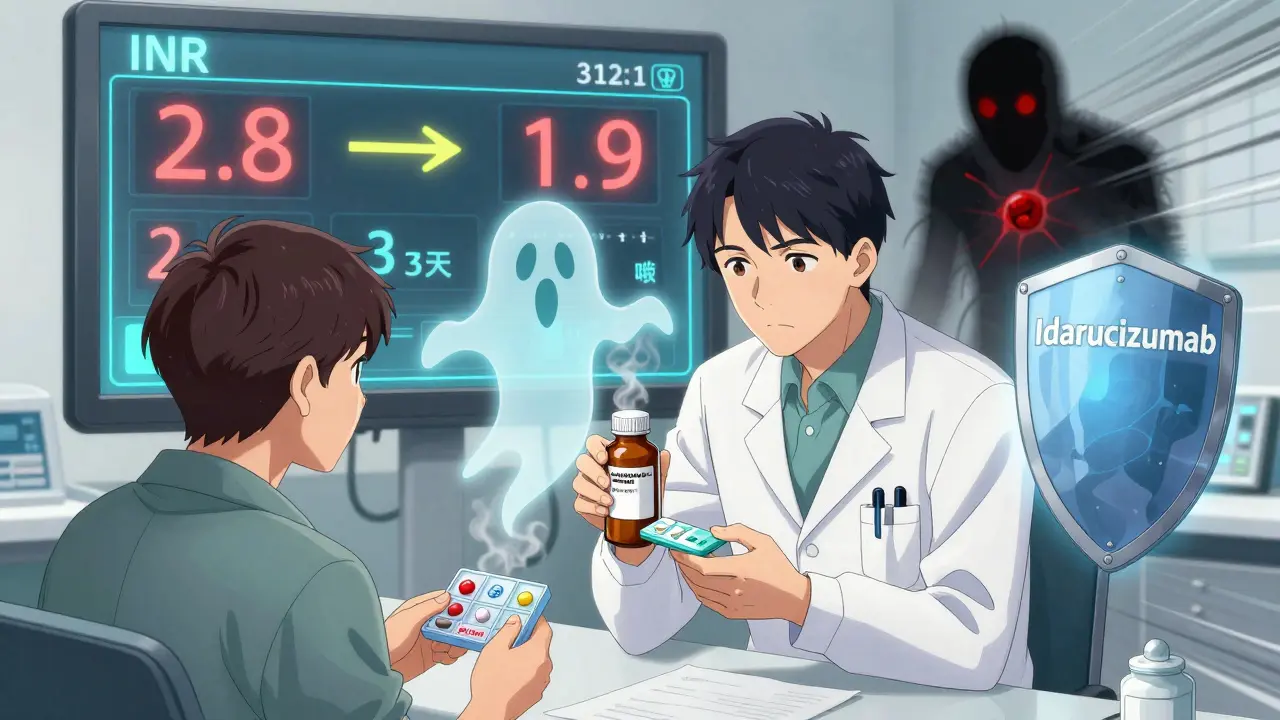
- INR ≤ 2.0: Start the DOAC right away.
- INR 2.0-2.5: Start the DOAC the same day or next day.
- INR 2.5-3.0: Wait 1-3 days, recheck INR.
- INR ≥ 3.0: Wait 3-5 days, recheck.
Which DOAC Should You Choose?
There are four main DOACs. They’re not all the same.- Dabigatran: Works by blocking thrombin. Must be stored in its original bottle-moisture ruins it. Not suitable for dosette boxes.
- Rivaroxaban, Apixaban, Edoxaban: These block Factor Xa. They’re more stable. Can go into pill organizers.
- CrCl 30-50 mL/min? You’ll likely need a lower dose.
- CrCl under 30? Most DOACs aren’t recommended.
Side Effects: What’s Different?
DOACs have fewer major side effects than warfarin. But they’re not side-effect-free.- Less intracranial bleeding: The RE-LY trial showed DOACs reduce brain bleeds by about 30% compared to warfarin.
- More GI bleeding: Especially with dabigatran. Stomach upset, nausea, or even bloody stools can happen. Not common, but more likely than with warfarin.
- No routine monitoring: That’s good-but risky if you miss doses. DOACs leave your system in 12-24 hours. Skip one, and you’re unprotected.
- Dabigatran: Can be reversed with idarucizumab.
- Rivaroxaban, apixaban, edoxaban: Can be reversed with andexanet alfa-but it’s expensive and not always available.
Special Situations: Surgery, Travel, and Kidneys
If you’re having surgery, you’ll need to stop your DOAC ahead of time. How long depends on your kidney function and the type of procedure. Example: A patient on dabigatran with CrCl = 90 mL/min having a low-risk procedure (like a dental extraction) should stop it 24-36 hours before. If CrCl is only 45 mL/min and it’s a major surgery? Stop 96-108 hours before. Travel? Bring extra pills. Don’t rely on refills abroad. Keep them in original packaging-especially dabigatran. Heat and humidity can ruin it. Kidney checks? Still needed. Every 6-12 months. DOACs are cleared by your kidneys. If your function drops, your drug builds up. That increases bleeding risk.What Your Doctor Should Do Before Switching
This isn’t something you should do on your own. Your doctor needs to:- Check your recent blood work: kidney function (CrCl), liver tests, full blood count-within the last 6 months.
- Measure your INR on the day of the switch.
- Calculate your creatinine clearance using the Cockcroft-Gault equation.
- Match the DOAC and dose to your kidney function, weight, and age.
- Give you written instructions on when to stop warfarin and when to start the DOAC.
- Provide an anticoagulant alert card and patient information leaflet.
What You Need to Do After the Switch
Once you’re on a DOAC:- Take it at the same time every day. No exceptions.
- Don’t stop it unless your doctor says so-even if you feel fine.
- Carry your anticoagulant alert card. Emergency staff need to know you’re on a blood thinner.
- Watch for signs of bleeding: unusual bruising, pink or red urine, black stools, headaches, dizziness.
- Call your doctor immediately if you fall hard, hit your head, or have unexplained pain.
- Keep your kidney tests on schedule.

Cost and Access
DOACs cost more. In the U.S., warfarin runs $10-$30 a month. DOACs? $500-$700. Insurance helps, but not always. In New Zealand, public funding covers some DOACs for eligible patients-check with your pharmacist. If cost is an issue, talk to your doctor. Sometimes switching back to warfarin is safer than skipping doses on a DOAC you can’t afford.What If You Need to Switch Back?
Sometimes, you might need to go back to warfarin. Maybe your kidney function dropped. Maybe you’re pregnant. Maybe your DOAC caused serious bleeding. Switching back is trickier. You can’t just start warfarin and expect it to work right away. It takes days to build up. So doctors often overlap DOACs with a short-term shot like heparin until the warfarin kicks in. This prevents clots during the transition.Final Thoughts
Switching from warfarin to a DOAC can be life-changing-fewer blood tests, fewer dietary limits, lower risk of brain bleeds. But it’s not automatic. It requires planning, precision, and partnership with your care team. The biggest danger isn’t the DOAC itself. It’s the gap in protection during the switch. Get the INR right. Time it right. Don’t skip doses. And never switch without medical supervision. If you’re considering this change, ask your doctor:- “Is my INR in the right range to switch?”
- “What’s my kidney function, and does it affect my dose?”
- “What do I do if I miss a pill?”
- “What signs of bleeding should I watch for?”
Can I switch from warfarin to a DOAC if I have atrial fibrillation?
Yes, most people with non-valvular atrial fibrillation are good candidates for switching to a DOAC. DOACs are actually preferred over warfarin in this group because they reduce the risk of stroke and brain bleeding. But you must have your INR checked before switching, and your kidney function must be adequate. If you have a mechanical heart valve, DOACs are not an option.
Do I still need blood tests after switching to a DOAC?
You won’t need INR tests anymore. But you still need kidney function tests-usually every 6 to 12 months. DOACs are cleared by your kidneys, so if your kidney function drops, the drug can build up and increase bleeding risk. Some doctors also check liver function or blood counts if you’re at higher risk.
What happens if I miss a dose of my DOAC?
If you miss a dose, take it as soon as you remember-unless it’s almost time for your next dose. Then skip the missed one. Never double up. DOACs leave your system in 12-24 hours. Missing a dose means your protection drops quickly. That’s why timing matters. Set phone reminders. Use a pill organizer-but not for dabigatran. Keep it in its original bottle.
Are DOACs safe during surgery or dental work?
Yes, but timing matters. For minor procedures like dental extractions, you might stop the DOAC 24-48 hours before. For major surgery, it could be 48-96 hours, depending on your kidney function and the DOAC you’re on. Always tell your surgeon or dentist you’re on a blood thinner. Your doctor will give you exact instructions based on your risk level and kidney health.
Can I take other medications while on a DOAC?
Many medications are safe, but some can increase bleeding risk. Avoid NSAIDs like ibuprofen or naproxen unless approved. Some antibiotics, antifungals, and seizure meds can interfere. Always check with your pharmacist before starting anything new-even over-the-counter supplements. Unlike warfarin, DOACs have fewer interactions, but they’re not immune.
Why is dabigatran stored differently than other DOACs?
Dabigatran is moisture-sensitive. If exposed to humidity, it can break down and lose effectiveness. That’s why it must stay in its original bottle with the desiccant. Other DOACs like rivaroxaban or apixaban are stable in pill organizers. Never transfer dabigatran to a dosette box-it could make your treatment unsafe.
Is switching to a DOAC worth the cost?
It depends. DOACs cost 20-50 times more than warfarin. But if you factor in the cost of frequent INR tests, emergency visits for bleeding, or strokes caused by poor control, the long-term savings can be real. For people who struggle with diet, alcohol, or remembering blood tests, DOACs offer better control and peace of mind. Talk to your doctor about your lifestyle and whether the benefits outweigh the cost for you.

Joe Bartlett
December 16, 2025 AT 14:31Jigar shah
December 18, 2025 AT 02:25Marie Mee
December 19, 2025 AT 08:31Philippa Skiadopoulou
December 20, 2025 AT 02:32Patrick A. Ck. Trip
December 20, 2025 AT 20:02Sam Clark
December 22, 2025 AT 19:12Virginia Seitz
December 24, 2025 AT 11:56amanda s
December 25, 2025 AT 21:57Brooks Beveridge
December 26, 2025 AT 07:53Anu radha
December 28, 2025 AT 02:13Jane Wei
December 29, 2025 AT 23:26Meghan O'Shaughnessy
December 30, 2025 AT 15:07Kaylee Esdale
December 31, 2025 AT 03:00Radhika M
December 31, 2025 AT 23:55