GI Bleeding Risk Calculator
Calculate Your Risk
Risk Assessment
Your Risk Factors
Current Annual Bleeding Risk
When you take an antidepressant from the SSRI class and a painkiller like ibuprofen at the same time, you’re stepping into a medical minefield. The combo can raise the chance of serious stomach bleeding by roughly three‑quarters compared with taking an NSAID alone. Below you’ll find why this happens, which patients are most vulnerable, and what you can do right now to stay safe.
Key Takeaways
- SSRIs + NSAIDs raise upper GI bleeding risk by ~75% (OR 1.75).
- Platelet serotonin blockade + mucosal injury = double‑hit mechanism.
- Older adults, prior ulcer history, and low‑dose aspirin users are highest‑risk groups.
- Proton pump inhibitors (PPIs) cut absolute bleeding risk by ~70%.
- Switching to acetaminophen or a COX‑2‑selective NSAID can eliminate the interaction.
Why the Combination Is Dangerous
Two separate processes converge when you mix SSRIs (selective serotonin reuptake inhibitors that lift mood by keeping serotonin in the brain) with NSAIDs (nonsteroidal anti‑inflammatory drugs that block COX enzymes and reduce pain)
- Platelet serotonin blockade: SSRIs stop platelets from pulling serotonin back into their granules. Without serotonin, platelets can’t clump together efficiently, weakening primary hemostasis.
- Mucosal injury: NSAIDs erode the stomach lining by inhibiting prostaglandin synthesis. Less prostaglandin means less mucus and bicarbonate, making the gut wall fragile.
When both mechanisms are present, a tiny ulcer can turn into a full‑blown bleed much faster than either drug would cause alone.
How Big Is the Risk?
Multiple meta‑analyses have converged on the same figure: an odds ratio of about 1.75 for upper GI bleeding when the two drug classes are used together. In plain language, that’s a 75 % jump over the risk of taking an NSAID by itself.
Some studies even reported a 12‑fold increase when a low‑dose aspirin was added to the mix - essentially the bleeding risk you’d expect from full‑strength anticoagulants.
Absolute numbers matter, too. In people over age 65 with a prior ulcer, the annual bleeding risk can climb from roughly 0.5 % to 1.5 % without any preventive steps.
Who’s Most at Risk?
- Age > 65 years
- History of peptic ulcer disease or GI surgery
- Concurrent low‑dose aspirin, clopidogrel, or warfarin
- High NSAID doses (e.g., >1,200 mg ibuprofen‑equivalent per day)
- Long‑term SSRI therapy (>90 days)
Even healthy younger adults aren’t immune; a large U.S. claims database showed about 13 % of adults on SSRIs also fill an NSAID prescription each year, creating a huge population‑wide exposure.
Preventive Strategies That Work
Guidelines from the American Gastroenterological Association (AGA) are crystal clear: anyone who absolutely needs both drug classes should be started on a proton pump inhibitor (PPI) right away.
| NSAID | COX Selectivity | Adjusted OR vs. SSRI‑only |
|---|---|---|
| Ibuprofen | Non‑selective (moderate) | 1.65 (95% CI 1.30‑2.09) |
| Naproxen | Non‑selective (high) | 1.82 (95% CI 1.40‑2.37) |
| Diclofenac | Non‑selective (high) | 1.90 (95% CI 1.45‑2.49) |
| Celecoxib | COX‑2 selective | 1.16 (95% CI 0.84‑1.61) |
| Acetaminophen | Not an NSAID | 1.00 (reference) |
Key take‑aways from the table:
- COX‑2‑selective agents like celecoxib carry the lowest added risk.
- Switching to acetaminophen removes the interaction entirely.
The AGA recommends a standard PPI dose of omeprazole 20‑40 mg daily (or equivalent). Real‑world data show this drops the absolute bleeding risk from about 1.5 % to 0.5 % per year-a 70 % relative reduction.
Step‑by‑Step Clinical Workflow
- Identify the combo. Flag any prescription or OTC record that contains an SSRI and an NSAID.
- Risk stratify. Use the AIMS65 score (Albumin, INR, Mental status, Systolic BP, Age > 65) plus history of ulcer disease.
- Explore alternatives. Ask if the patient can switch to acetaminophen or a topical NSAID for pain.
- Start a PPI. If the NSAID must stay, prescribe a PPI immediately.
- Educate. Explain the bleeding warning, signs of melena or hematemesis, and when to seek care.
- Document. Write a concise note in the electronic health record noting the interaction and the preventive plan.
Clinician education programs that embed these steps have cut inappropriate SSRI‑NSAID prescribing from 28 % to under 10 % in several health systems.
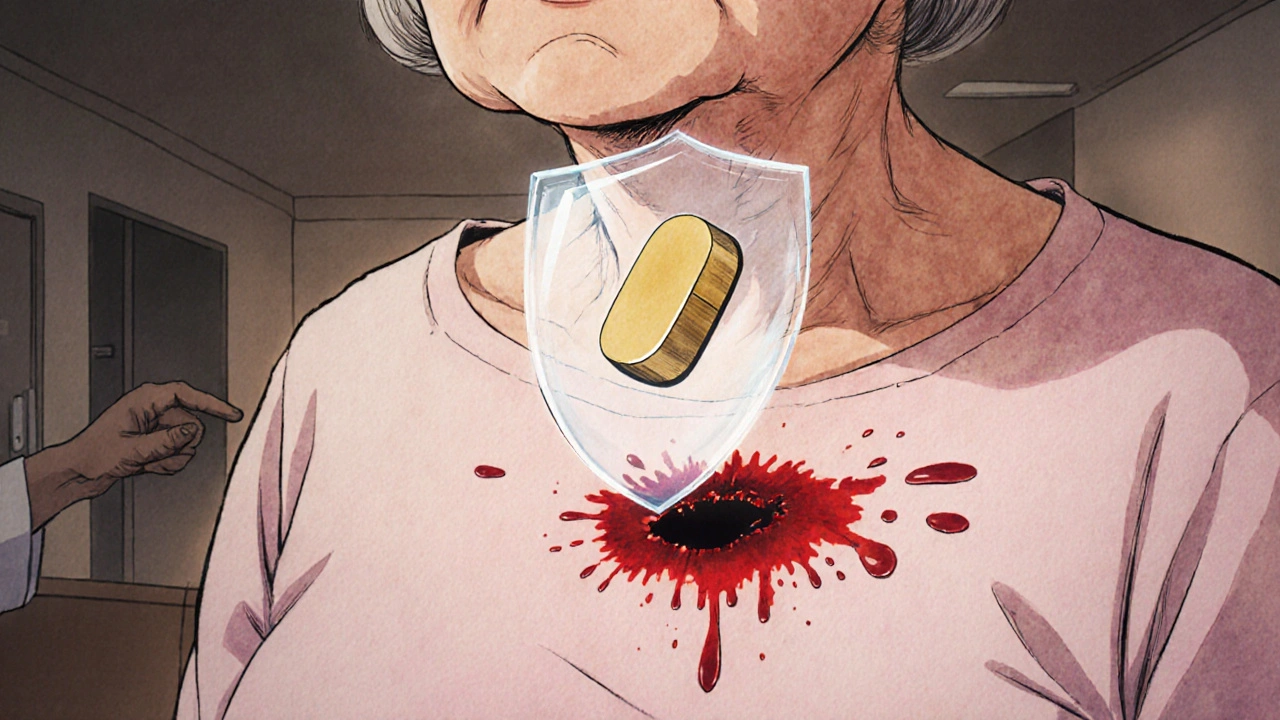
Patient Stories That Highlight the Issue
On a popular drug‑review site, a user named "MidwestMom" recounted a six‑month stretch of sertraline plus ibuprofen that ended in an ER visit for stomach bleeding. Her doctor had never mentioned the risk. In contrast, another poster, "AnxietyFree," said her doctor swapped naproxen for acetaminophen when she started fluoxetine, and she’s been bleed‑free for two years.
These anecdotes mirror the data: many patients learn the hard way, but proactive management prevents most events.
Future Directions and Emerging Tools
New risk calculators, like the GI‑BLEED tool integrated into Epic, pull 12 variables-including the specific SSRI and NSAID, genetic CYP2C19 status, and comorbidities-to give a personalized bleeding probability. Early validation shows 89 % accuracy, and hospitals that have adopted the tool report a 30 % drop in bleeding admissions.
Research is also probing SSRI alternatives with a cleaner platelet profile. Vortioxetine, for example, showed a 40 % lower bleeding rate in a phase‑4 trial, while novel agents such as lumateperone are still in early development.
Regulators are catching up, too. The FDA’s 2023 Sentinel Initiative will follow half a million patients on these combos to fine‑tune labeling and decision‑support mandates. By 2030, experts expect a 60 % reduction in inappropriate co‑prescribing.
Bottom Line Checklist
- Never start an SSRI in a patient who is regularly taking a non‑selective NSAID without checking bleeding risk.
- If the combo is unavoidable, prescribe a PPI and monitor for GI symptoms.
- Consider acetaminophen or a COX‑2‑selective NSAID as first‑line pain relief for patients on SSRIs.
- Document the interaction in the EHR; alerts can cut events by a third.
- Re‑evaluate therapy every 3‑6 months, especially in older adults.
Does every SSRI increase bleeding risk the same amount?
Paroxetine and fluoxetine are the strongest serotonin‑reuptake blockers, so they tend to raise risk a bit more than sertraline or citalopram. The difference isn’t huge, but if a patient is high‑risk, choosing a weaker SSRI can shave a few percent off the absolute bleed probability.
Can over‑the‑counter ibuprofen be taken safely with an SSRI?
It’s not “safe” in the strict sense. Even OTC doses increase bleeding odds. If the patient needs occasional pain relief (< 2 days), the risk is low, but regular use (> 3 days/week) should trigger a PPI or a switch to acetaminophen.
Do PPIs completely eliminate the danger?
PPIs dramatically lower the risk-by about 70 %-but they don’t erase it. Patients still need to watch for dark stools or vomiting blood, especially if they add aspirin or have a prior ulcer.
Is there a cheap over‑the‑counter PPI I can recommend?
Omeprazole 20 mg daily is widely available for around $0.15 a pill. Many pharmacies also stock generic lansoprazole, which works equally well.
What if a patient is already on low‑dose aspirin?
Add a PPI and consider switching the NSAID to celecoxib or, better yet, acetaminophen. The triple combo (SSRI + NSAID + aspirin) pushes bleeding risk into the same range as full‑strength anticoagulation.

Max Lilleyman
October 24, 2025 AT 22:12Mixing SSRIs with ibuprofen? Bad idea 😑
Brett Witcher
October 26, 2025 AT 04:00The pharmacodynamic interaction between serotonergic reuptake inhibition and cyclooxygenase blockade constitutes a synergistic attenuation of hemostasis.
Empirical data indicate a 1.75‑fold increase in upper gastrointestinal hemorrhage incidence.
Accordingly, clinicians should preemptively prescribe a proton pump inhibitor when co‑administration is unavoidable.
Benjamin Sequeira benavente
October 27, 2025 AT 10:48Listen up, anyone still popping a daily ibuprofen while on an SSRI needs a reality check.
First, serotonin isn’t just a mood chemical; it’s a critical player in platelet aggregation.
When you block its reuptake, platelets lose the ability to clump efficiently, leaving the clotting cascade compromised.
Second, NSAIDs chew away the protective mucus lining of your stomach by throttling prostaglandin synthesis.
Combine those two hits and you’ve got a perfect storm for a bleeding ulcer.
The odds ratio sits around 1.75, meaning a 75 % jump in risk compared with NSAIDs alone.
For patients over 65 or with a history of ulcers, that translates to a jump from 0.5 % to 1.5 % annual bleed risk.
If you add low‑dose aspirin into the mix, you’re flirting with the same bleed rates as full‑strength anticoagulants.
What does that mean in plain language? One missed dose could become a trip to the ER with melena or hematemesis.
The good news: a standard dose of a PPI slashes that absolute risk by about 70 %.
So if you absolutely must take both, start a PPI yesterday.
Even better, switch the NSAID to a COX‑2‑selective agent like celecoxib, or ditch the NSAID entirely in favor of acetaminophen.
Acetaminophen carries essentially zero additive bleed risk when paired with an SSRI.
Don’t forget to reassess therapy every three to six months, especially in older adults.
Educate patients to watch for dark stools, vomiting blood, or unexplained fatigue.
Document the interaction in the electronic health record; alerts can cut events by a third.
Bottom line: avoid the combo when possible, protect with a PPI when not, and keep a close eye on high‑risk patients.
Shannon Stoneburgh
October 28, 2025 AT 17:36Serotonin helps platelets form clots, and NSAIDs damage the stomach lining, so together they raise bleed risk.
Older people and those with past ulcers should be especially careful.
Nathan Comstock
October 30, 2025 AT 00:24This isn’t a minor inconvenience, it’s a battlefield inside your gut!
When you mash an SSRI with ibuprofen you’re basically declaring war on your own stomach wall.
Every day you do it you’re inviting a catastrophic bleed that could land you in the ICU.
Don’t be fooled by “just a little painkiller” - the consequence is nothing short of a medical disaster.
Terell Moore
October 31, 2025 AT 07:12Oh sure, because ignoring decades of pharmacology research always ends well.
Why not add a third drug while you’re at it?
Amber Lintner
November 1, 2025 AT 14:00Maybe the risk is overblown; many people take both without any drama.
Olivia Harrison
November 2, 2025 AT 20:48Hey there! You’re right, the combo can be risky, but there are practical steps to stay safe.
First, if you need pain relief, try acetaminophen before reaching for ibuprofen.
If NSAIDs are unavoidable, a once‑daily PPI like omeprazole can dramatically lower the bleed risk.
Second, keep an eye on any dark stools or unexplained fatigue and call your doctor early.
Lastly, discuss with your prescriber about possibly switching to a COX‑2‑selective NSAID if you must stay on an SSRI.
Abhinav B.
November 4, 2025 AT 03:36In India we see a lot of self‑medication with over‑the‑counter painkillers, and many patients aren’t aware of the SSRI‑NSAID interaction.
Even with the best guidelines, the real‑world adherence is low.
Encouraging pharmacists to flag this combo could save many lives.
Plus, generic PPIs are affordable, so cost isn’t a big barrier.
Abby W
November 5, 2025 AT 10:24That’s spot on! 👍 It’s easy to forget how platelets need serotonin.
Also, reminding patients to take PPIs with food can improve adherence.
Keep spreading the word! 😊
Grace Silver
November 6, 2025 AT 17:12Philosophy teaches us that unseen forces shape our health, much like the invisible serotonin in platelets.
When we neglect those forces, consequences rise like tides.
Thus, awareness becomes an ethical duty.
Act now, think later.
Tamara Schäfer
November 8, 2025 AT 00:00True, the drama is real, but there’s also hope.
By swapping ibuprofen for acetaminophen or adding a PPI, you can dodge most of the blood‑shed drama.
Stay proactive and keep the conversation with your doctor open.
Optimism plus smart choices = safer outcomes.
Corrine Johnson
November 9, 2025 AT 06:48Honestly, the data are crystal‑clear, - mixing SSRIs with non‑selective NSAIDs without gastro‑protective therapy is reckless, - especially in the elderly, - and it’s high time clinicians stop treating this as an optional risk.