When you’re managing medications, knowing the difference between brand names and generics can save you hundreds of dollars a year. But if you speak Spanish and don’t have access to clear, reliable information in your language, that savings can slip through your fingers - not because you don’t want to save money, but because you’re confused about what you’re taking.
What Exactly Is a Generic Medication?
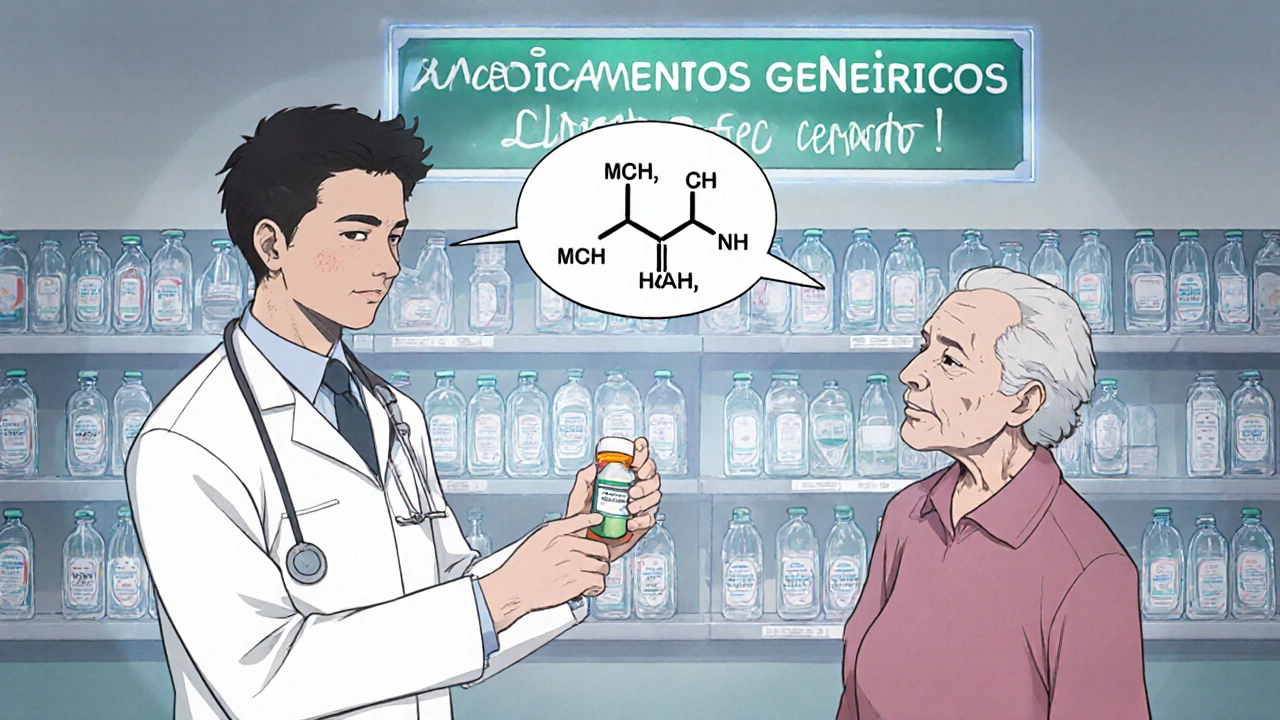
In English, we say "generic medication." In Spanish, it’s el medicamento genérico. That’s the first thing you need to know. It’s not a cheaper version of the real medicine - it’s the exact same medicine. Same active ingredient. Same dose. Same effect. The only differences are the color, shape, or name on the pill, and the price.
Many Spanish-speaking patients stop taking their meds because they think the generic looks different, so it must be weaker. One patient in Texas told his doctor: "La pastilla es de otro color, no es la misma." (The pill is a different color - it’s not the same.) But that’s normal. Generic pills look different because they’re made by different companies. The FDA requires them to work the same way, but doesn’t require them to look identical.
Why This Matters: Cost, Compliance, and Safety
Nine out of ten prescriptions in the U.S. are filled with generics. Yet only about one in three Spanish-speaking patients fully understand that generics are just as safe and effective as brand names. That’s a huge gap.
Why? Because the cost difference is real. A brand-name blood pressure pill might cost $150 a month. The generic? $12. That’s $1,500 a year saved. But if you don’t trust the generic because you don’t understand it, you might skip doses, stop taking it, or switch back to the expensive version - and your health suffers.
Studies show that when Spanish-speaking patients get clear, visual explanations about generics, they’re 37% more likely to stick with them. That’s not just about money - it’s about keeping chronic conditions under control: diabetes, high blood pressure, cholesterol, asthma.
Where to Find Trusted Spanish-Language Resources
Not all Spanish materials are created equal. Some are poorly translated. Others use confusing regional terms. Here are the most reliable sources right now:
- Agency for Healthcare Research and Quality (AHRQ) - Their "My Medicines List" is available in Spanish and asks you to write down both the brand name and generic name of each medicine, why you take it, the dose, and how often. It’s simple, practical, and updated through December 2024.
- MedlinePlus.gov - Offers a bilingual PDF comparing brand and generic names side by side. It includes common medications like metformin (Glucophage), lisinopril (Zestril), and atorvastatin (Lipitor).
- Wake AHEC Pharmacy Translation Card - Designed for healthcare workers, but useful for patients too. It includes phrases like: "Esta medicina tiene una apariencia diferente, pero es lo mismo." (This medicine looks different, but it’s the same.)
- NIH’s "Medicamento Genérico" App - Launched in September 2023, this free app lets you scan a pill, see its brand and generic name, compare images of different versions, and even hear the correct pronunciation of drug names in Spanish.
- Spanish Academy’s Pharmacy Vocabulary Guide - Lists 27 essential terms like "medicamentos de venta libre" (over-the-counter medicines) and "receta médica" (prescription). Updated monthly.
Common Spanish Phrases You Should Know
If you’re going to talk to your pharmacist or doctor, these phrases will help you get the right information:
- "¿Tiene la versión genérica de esa medicina?" - Do you have the generic version of that medicine?
- "¿Es lo mismo que la marca?" - Is it the same as the brand?
- "¿Por qué se ve diferente?" - Why does it look different?
- "¿Puedo usar esta versión para ahorrar dinero?" - Can I use this version to save money?
- "¿Esta pastilla tiene el mismo ingrediente activo?" - Does this pill have the same active ingredient?
And if you’re ever unsure, ask: "¿Puede mostrarme una imagen de cómo se ve la versión genérica?" - Can you show me a picture of what the generic looks like?
Regional Differences: Paracetamol vs. Acetaminofén
Here’s where things get tricky. The same drug can have different names depending on where you’re from. In Spain, "paracetamol" is common. In Mexico, Colombia, and most of Latin America, it’s called "acetaminofén." But it’s the same pill. Same effect. Same safety profile.
This confusion leads to real problems. A patient in California might get prescribed "acetaminofén" at her local clinic. Then she travels to Arizona and hears her new pharmacist say "paracetamol." She thinks it’s a new drug - and refuses to take it.
That’s why the best resources now include regional variations. The NIH app and updated AHRQ materials list both names side by side. Always ask: "¿Se llama diferente en otros países?" - Is it called something else in other countries?

What Patients Are Saying - Real Stories
On Reddit, a user named Rosa wrote: "Mi papá dejó de tomar su medicina para la presión porque la pastilla era azul en vez de roja. Pensó que ya no funcionaba. Nosotros no sabíamos que los genéricos cambian de color. Ahora uso la app del NIH y él toma sus pastillas otra vez."
A nurse in Los Angeles shared: "I’ve had patients cry because they thought switching to a generic meant their doctor didn’t care. I show them the FDA logo on the bottle - that’s the stamp that says it’s safe. Then I show them the price difference. It changes everything."
And a survey from the California Health Care Foundation found that 78% of Spanish-speaking patients felt more confident using generics after seeing bilingual visuals - but 63% still worried they weren’t as strong. That’s the gap we still need to close.
What’s Missing - And What’s Coming
Most free resources still don’t explain why generics are safe. They don’t mention that the FDA requires them to be within 3-5% of the brand’s effectiveness. They don’t show side-by-side photos of the same drug from different makers. They don’t play audio of how to pronounce "metoprolol" or "levothyroxine" correctly.
That’s changing. In early 2024, Kaiser Permanente rolled out a Spanish portal with video clips of pharmacists explaining generics in Mexican, Puerto Rican, and Colombian Spanish. Epic Systems, the big EHR company, is now testing AI tools that automatically generate personalized Spanish explanations based on where a patient was born.
And the demand is growing. The U.S. Hispanic population will hit 111 million by 2060. More people need clear, accurate, and culturally relevant info - not just translated brochures.
How to Use These Resources Right
Here’s what works:
- Ask your pharmacist: "¿Tiene la versión genérica?" - Always ask. It’s your right.
- Use the NIH app to scan your pill and see what it looks like in other versions.
- Keep a printed copy of AHRQ’s "My Medicines List" in Spanish. Fill it out with your doctor.
- If a pill looks different than last time, don’t assume it’s wrong. Ask: "¿Es la misma medicina, solo diferente apariencia?"
- Share these tools with family. Many older adults rely on their kids to explain meds - make sure they understand too.
Generic medications aren’t second-rate. They’re the smart choice. And with the right tools in Spanish, you can take control - without paying more than you have to.
Are generic medications as safe as brand-name drugs in Spanish-speaking patients?
Yes. The U.S. Food and Drug Administration (FDA) requires generic medications to contain the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict standards for purity, stability, and performance. Studies show no difference in effectiveness or safety between generics and brand-name drugs for the vast majority of medications. The only differences are in inactive ingredients - like color or filler - which don’t affect how the medicine works.
Why do generic pills look different from brand-name ones?
Generic pills look different because U.S. law requires them to have a distinct appearance from the brand-name version to avoid trademark infringement. That means different colors, shapes, or markings - but not different effects. For example, the brand-name drug Lipitor (atorvastatin) is blue, while the generic version might be white or yellow. This confuses many patients who think a different color means a different drug. Resources like the NIH’s "Medicamento Genérico" app show side-by-side images to help patients recognize that the change is normal.
What’s the difference between "paracetamol" and "acetaminofén"?
They’re the same drug. "Paracetamol" is the term used in Spain and some parts of Europe. "Acetaminofén" is used in Latin America and the U.S. Spanish-speaking communities. The chemical compound is identical: C8H9NO2. It’s used for pain and fever. If you move between regions or see different names on prescriptions, don’t assume it’s a different medicine. Always check the active ingredient listed on the label.
Can I trust free Spanish-language resources from the internet?
Some can, but not all. Stick to trusted sources like the U.S. government (AHRQ, MedlinePlus, NIH), major medical associations, or university health systems. Avoid blogs, social media posts, or apps without clear authorship or citations. Many poorly translated resources use incorrect terms or oversimplify complex concepts. For example, some say "la medicina genérica es más débil" - which is false. Always cross-check with official materials or ask your pharmacist to confirm.
How can I help my elderly parent understand generic medications in Spanish?
Start with visuals. Use the NIH app to show them side-by-side images of the brand and generic versions. Print out AHRQ’s "My Medicines List" in Spanish and fill it out together. Read the instructions aloud and ask them to repeat back what they understand. Use simple phrases like: "Es la misma medicina, solo diferente color" (It’s the same medicine, just different color). Avoid medical jargon. If they’re still unsure, ask their pharmacist to explain it in person - many pharmacies now offer free bilingual counseling.
Do pharmacies in the U.S. offer free Spanish-speaking pharmacists?
Many do - especially large chains like CVS, Walgreens, and Kaiser Permanente. Some community pharmacies hire bilingual staff. But not all do. If you don’t see a Spanish-speaking pharmacist, ask if they have access to a live interpreter or video translation service. Under federal law (Section 1557 of the Affordable Care Act), healthcare providers must offer language assistance at no cost. You have the right to ask for help in your language - no matter where you are.


dayana rincon
November 28, 2025 AT 14:38Charity Peters
November 29, 2025 AT 23:53Chelsey Gonzales
November 30, 2025 AT 11:54Sarah Khan
December 1, 2025 AT 20:20Tressie Mitchell
December 2, 2025 AT 18:50Faye Woesthuis
December 2, 2025 AT 21:15MaKayla Ryan
December 3, 2025 AT 22:34Kelly Yanke Deltener
December 5, 2025 AT 06:49Cindy Burgess
December 6, 2025 AT 02:32Orion Rentals
December 7, 2025 AT 13:36Sondra Johnson
December 8, 2025 AT 20:33Crystal Markowski
December 10, 2025 AT 06:47Kelly Library Nook
December 11, 2025 AT 11:52raja gopal
December 13, 2025 AT 07:32