When you think of Parkinson’s disease, you probably picture a shaking hand. But that’s just the tip of the iceberg. Parkinson’s is a slow, creeping condition that changes how your body moves, how you speak, and even how you live day to day. It doesn’t just affect older people - about 4% of cases show up before age 50. And while there’s no cure yet, knowing what to expect and how to manage it can make a huge difference in staying independent longer.
What You’ll Feel: The Four Main Motor Symptoms
The core signs of Parkinson’s are four motor symptoms that doctors look for when making a diagnosis. You don’t need all four, but you almost always have at least one - and bradykinesia is the one you can’t miss. It means slow movement. Not just slow walking. Slow everything. Getting out of bed, buttoning a shirt, brushing your teeth. What used to take 10 seconds now takes 30. Studies show people with Parkinson’s take 2.3 times longer to dress and 3.1 times longer to button a shirt compared to someone their age without the disease.
Then there’s rigidity. Your muscles feel stiff, like they’re wrapped in rubber bands. Sometimes it’s a constant resistance - called lead-pipe rigidity. Other times, it’s a jerky, ratchety feel - cogwheel rigidity - when someone moves your arm. About 85% of people with Parkinson’s get this. It’s why you might feel like your arms are heavy or why turning over in bed becomes a chore. Around 65% of people report trouble rolling over within five years of diagnosis.
Tremor is what most people think of first. That pill-rolling motion between thumb and finger. It usually starts on one side only - maybe your right hand while you’re sitting still. It fades when you move your hand to pick up a cup. About 70% of people have tremor at diagnosis, but 20-30% never get it. So if you don’t shake, it doesn’t mean you don’t have Parkinson’s. Bradykinesia is the real clue.
Finally, postural instability shows up later. This is when your balance starts to go. You lean forward, you stumble when you turn, you fall more often. About 68% of people with Parkinson’s fall at least once a year. One in three fall repeatedly. This isn’t just clumsiness - it’s your brain losing its ability to adjust your posture quickly. It usually appears after five to ten years, but when it does, it changes everything.
Other Motor Signs You Might Not Notice
There’s more than just the big four. You might not realize these are part of Parkinson’s until someone points them out.
- Reduced arm swing: When you walk, one or both arms don’t swing like they used to. It’s subtle, but it throws off your balance. About 75% of people lose this natural rhythm.
- Stooped posture: You start leaning forward, shoulders rounded. It’s not just bad posture - it’s your muscles tightening in a way that pulls you down. Seen in 65-80% of patients.
- Micrographia: Your handwriting gets smaller and smaller. Lines crowd together. You might not notice it yourself, but family members do.
- Soft voice: Your voice drops in volume. On average, it’s 5-10 decibels quieter. That’s like speaking from another room. People ask you to repeat yourself constantly.
- Drooling: You’re not swallowing as often. Saliva builds up. It’s not because you’re messy - it’s because your swallowing reflex is slowed. Affects 50-80% of people.
- Dysphagia: Swallowing food or pills becomes hard. In advanced stages, up to 80% struggle with this. That’s dangerous - it leads to aspiration pneumonia, which causes 70% of Parkinson’s-related deaths.
- Dystonia: Muscles cramp or twist painfully. Often seen in young-onset cases. Toes curl, feet turn inward. It can happen at night or after taking medication.
Medications: What Works, What Doesn’t, and What Comes Next
There’s no drug that stops Parkinson’s from getting worse. But there are drugs that help you feel better - for a while.
Levodopa is the gold standard. It’s what your brain turns into dopamine - the chemical your neurons stopped making. It works for 70-80% of people at first. You feel more like yourself. Walk easier. Speak louder. But after five years, up to half of people start having problems: the medicine doesn’t last as long, or you get sudden, jerky movements called dyskinesias. That’s not the disease getting worse - it’s the medicine’s side effect.
For younger patients, doctors often start with dopamine agonists like pramipexole or ropinirole. These mimic dopamine without turning into it. They’re less powerful than levodopa, helping about 50-60% of early-stage patients. But they can cause side effects like nausea, dizziness, or even compulsive behaviors - gambling, shopping, or hypersexuality. That’s why they’re usually saved for people under 60.
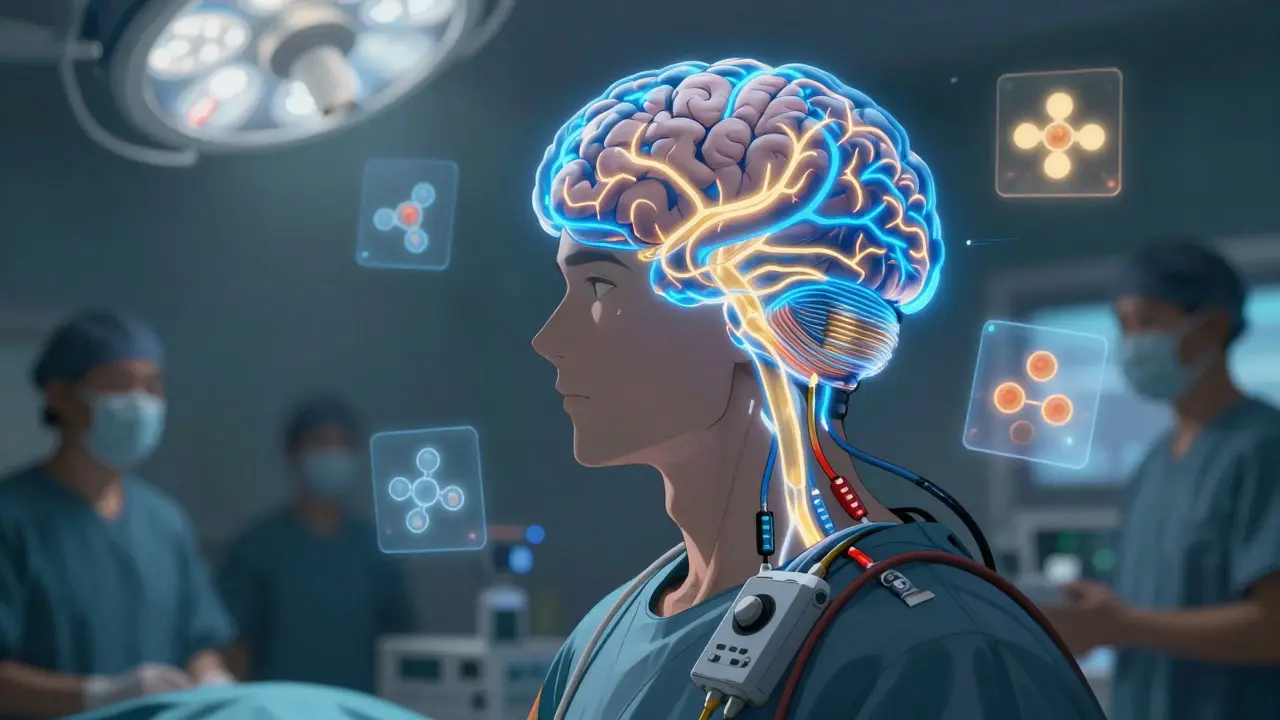
After ten years, about 30% of people need deep brain stimulation (DBS). It’s surgery. Electrodes are placed in specific parts of the brain, connected to a pacemaker-like device in the chest. It doesn’t cure anything, but it smooths out the ups and downs of medication. People who get it often reduce their pill dose by half and have fewer dyskinesias.
There are other pills too - MAO-B inhibitors like selegiline, COMT inhibitors like entacapone - they’re usually added on to levodopa to make it last longer. But none of them stop the disease. They just help you manage it.
Living With Parkinson’s: The Everyday Battle
It’s not just about meds and movements. It’s about how you live.
Walking becomes a minefield. Step length drops by 25-35%. Walking speed slows by 30-40%. That’s why falls happen. You don’t just lose balance - you lose confidence. Many people stop going out because they’re afraid of falling.
Simple tasks take forever. Getting dressed, cooking, bathing - they all need more time and planning. Some people start using adaptive tools: button hooks, weighted utensils, non-slip mats. Occupational therapists can help you find what works.
Sleep gets messy. You might kick out in your sleep. You might feel restless all night - a condition called akathisia. It affects 15-25% of people and makes exhaustion worse. Others can’t get comfortable because of stiffness or cramps.
Sexual health often drops off. For men, erectile dysfunction affects 50-80%. It’s not just physical - it’s psychological. The disease, the meds, the stress - it all adds up. No one talks about it, but it’s real.
And then there’s the voice. You start speaking softly. People misunderstand you. You stop joining conversations. You feel isolated. Speech therapy helps. Singing exercises, loud voice training - they can bring back volume and clarity.
What Actually Helps: Exercise, Therapy, and Support
Medication isn’t the only tool. Movement is medicine.
Studies show 12 weeks of targeted exercise - tai chi, dance, boxing, even brisk walking - improves walking speed by 15-20% and cuts fall risk by 30%. Physical therapy isn’t optional. It’s essential. It teaches you how to turn safely, how to stand up from a chair without leaning forward, how to take bigger steps.
Speech therapy isn’t just for people who can’t be heard. It helps with swallowing too. Swallowing exercises reduce the risk of choking and pneumonia.
Occupational therapy helps you adapt your home. Grab bars, raised toilet seats, rocker knives, voice-activated lights - small changes that add up to independence.
And don’t underestimate the power of community. Support groups, online forums, Parkinson’s foundations - they give you more than advice. They give you back your sense of normalcy.
Where Things Stand Today
Parkinson’s still progresses. No drug has proven it can slow or stop the brain cell loss. Research is chasing alpha-synuclein - the protein that clumps in Parkinson’s brains - but so far, nothing has worked in large trials.
But here’s the good part: we know more now than ever about how to live well with it. People diagnosed today can expect to live for decades. With the right combination of meds, therapy, and support, many stay active, engaged, and independent for years longer than they thought possible.
The goal isn’t to cure it. It’s to live fully while you have it.
Is tremor always the first sign of Parkinson’s?
No. While tremor is the most common symptom at diagnosis - seen in about 70% of cases - 20-30% of people never develop it. The one symptom you almost always have is bradykinesia, or slow movement. If you’re noticing you’re slower to get up, button shirts, or write, that’s a bigger red flag than shaking.
Can Parkinson’s be diagnosed with a scan or blood test?
No. There’s no blood test or MRI that confirms Parkinson’s. Diagnosis is based on clinical signs: a neurologist looks for bradykinesia plus either tremor or rigidity. A strong response to levodopa also supports the diagnosis. Some scans can rule out other conditions, but they can’t confirm Parkinson’s.
Why does levodopa stop working after a few years?
Levodopa doesn’t stop working - your brain’s ability to store and release dopamine does. As more dopamine-producing cells die, your brain can’t smooth out the drug’s effects. This leads to "on-off" fluctuations, where you suddenly switch from moving well to being frozen. It can also cause dyskinesias - involuntary jerks. That’s why doctors delay levodopa in younger patients or add other meds to stretch its effect.
Is deep brain stimulation a cure?
No. DBS doesn’t stop Parkinson’s from progressing. It helps control motor symptoms - especially tremor, stiffness, and medication fluctuations - by sending electrical pulses to specific brain areas. It’s most effective for people who still respond to levodopa but have unpredictable side effects. It doesn’t help with speech, balance, or non-motor symptoms like depression or memory.
Can exercise really make a difference?
Yes. Exercise isn’t just good for you - it’s one of the most effective tools for managing Parkinson’s. Studies show 12 weeks of regular activity improves walking speed by 15-20% and reduces falls by 30%. Activities that challenge balance and coordination - like tai chi, dance, or boxing - are especially helpful. The key is consistency. It’s not about intensity; it’s about showing up.
What’s the biggest risk to life with Parkinson’s?
The biggest risk isn’t the disease itself - it’s complications. Swallowing problems (dysphagia) lead to aspiration pneumonia, which causes about 70% of Parkinson’s-related deaths. Falls are another major danger. Managing swallowing with therapy and preventing falls with home modifications and balance training are critical for long-term safety.


Shelby Marcel
January 24, 2026 AT 13:09i had no idea micrographia was a thing lol my dad’s handwriting got so tiny last year i thought he was just being lazy
Juan Reibelo
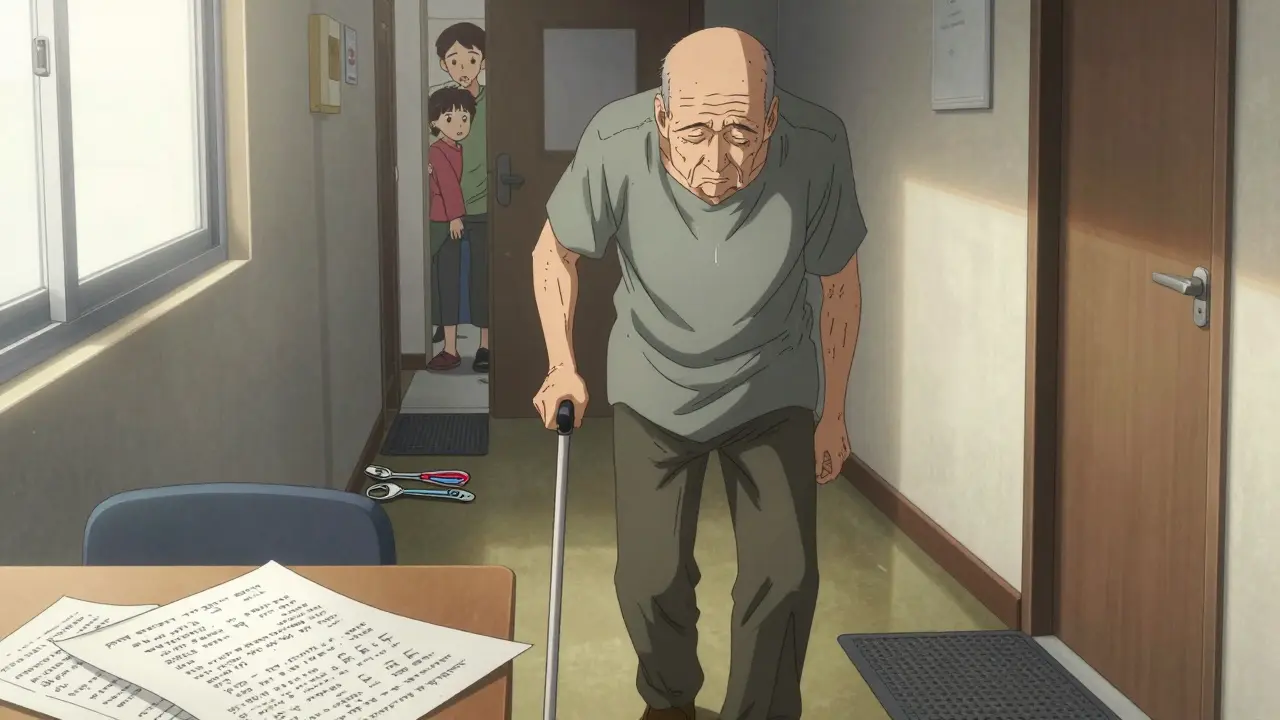
January 26, 2026 AT 04:11Bradykinesia is the silent thief. You don’t notice it until you’re standing in front of the fridge, and it takes you seven minutes to decide what to eat-because your brain is still processing the thought of opening the door. And then you forget why you opened it.
I’ve seen it in my uncle. He used to fix cars. Now he can’t twist a jar lid without stopping three times to breathe. No tremor. No drama. Just… slow. So slow.
People say, ‘Just move faster!’ Like it’s a choice. It’s not. It’s like your limbs are underwater, and someone keeps turning up the viscosity.
And the worst part? You’re the only one who feels it. To everyone else, you’re just ‘being lazy’ or ‘getting old.’
But here’s the thing: he still plays chess every Sunday. Takes him 45 minutes to make a move. But he makes it. And that’s the victory.
Medication helps. But presence? Presence is the real treatment.
I don’t know why this post hit me so hard. Maybe because I’m watching someone I love become a ghost in slow motion.
And I’m just here… watching.
Luke Davidson
January 27, 2026 AT 16:24Just wanna say thank you for writing this. My mom was diagnosed 3 years ago and this is the first time I’ve read something that actually explained what’s happening inside her body-not just the ‘shaky hand’ stuff they show on TV.
We started doing tai chi together last winter. She hates it at first. Now she says it’s the only time she feels like herself. Not a patient. Not a burden. Just… her.
And yeah, she drools now. We got those absorbent collars. No shame. No stigma. Just life.
Also-speech therapy changed everything. She sings along to old Motown records now. Loud as hell. Neighbors love it.
You’re not alone. Even on the days it feels like you are.
Patrick Gornik
January 28, 2026 AT 03:11Let’s be real: Parkinson’s isn’t a disease-it’s a systemic failure of neurobiological entropy management. Your dopaminergic neurons are basically the last holdouts of a collapsing cortical empire, and levodopa? It’s just a temporary patch job on a leaking dam made of alpha-synuclein tar.
We’re treating symptoms like they’re the root cause, while the real villain-the misfolded protein cascade-gets a free pass because Big Pharma doesn’t want to fund trials that might actually work.
And don’t get me started on DBS. It’s neurosurgical theater. You’re not curing anything-you’re just hacking the basal ganglia like a BIOS override. It’s like putting a turbo button on a sinking ship.
Meanwhile, exercise is the only ‘treatment’ that doesn’t come with a patent. That’s not medicine. That’s rebellion.
And yet, we keep pretending this is a medical problem instead of a societal one. We medicate instead of mobilize. We isolate instead of integrate.
The real tragedy? We’ve known for decades that movement is neuroprotective. But we’d rather hand out pills than build sidewalks.
So yes-exercise helps. But it’s not a cure. It’s a protest.