One in three women over 50 will break a bone because of weak bones. One in five men over 50 will too. And most of them had no idea their bones were crumbling until it was too late. Osteoporosis doesn’t come with pain, swelling, or warning signs. It sneaks in silently, stealing strength from your skeleton until a simple stumble turns into a broken hip, a crushed spine, or worse. The good news? You can stop it - if you know what to do.
Why Your Bones Are Losing Strength
Your bones aren’t static. They’re alive, constantly breaking down and rebuilding. Until about age 30, your body builds more bone than it loses. That’s your peak bone mass. After that, the balance shifts. You lose a little each year - about 0.3% to 0.5%. But for women after menopause, that rate jumps to 2% to 3% a year for the first five to seven years. That’s not just aging. That’s a biological earthquake. Men lose bone too, but slower. Why? Women start with less bone mass to begin with, and when estrogen drops, the body’s bone-building system slows down fast. Men with low testosterone face similar risks. Age isn’t the only culprit. Genetics play a huge role. If your mom or dad broke a hip after 50, your risk goes up by 60% to 80%. White and Asian women are at higher risk than Black or Hispanic women. And if you had early menopause - before 45 - your odds of fracture jump 2.1 times.The Hidden Triggers You Can Control
Not everything about osteoporosis is written in your DNA. Many of the biggest risks are habits you can change. And fixing them doesn’t require magic pills or expensive treatments. Calcium isn’t optional. Adults under 50 need 1,000 mg a day. After 50, you need 1,200 mg. But most people get less than half that. Dairy isn’t the only source. Canned salmon with bones, kale, bok choy, fortified plant milks, and tofu set in calcium sulfate all count. If you can’t get enough from food, supplements help - but don’t take more than 500-600 mg at once. Your body can’t absorb more. Spread it out with meals. Vitamin D is the key that unlocks calcium. Without it, your body can’t use the calcium you eat. Over 40% of U.S. adults are deficient. You need 800-1,000 IU daily. If your levels are below 20 ng/mL, you may need 2,000 IU for a few months to catch up. Sunlight helps, but in winter or if you’re indoors most of the day, supplements are your best bet. Smoking cuts your bone density by 55%. It messes with estrogen, blocks calcium absorption, and kills bone-building cells. Quitting doesn’t reverse all the damage, but it stops the bleeding. Every year you stay smoke-free, your bones get a little stronger. Alcohol is a bone killer. More than two drinks a day increases hip fracture risk by 41%. That’s not just heavy drinking - it’s two glasses of wine or two beers daily. Cut back. Even one drink a day is safer than two. Sitting is the silent thief. If you don’t put stress on your bones, they forget how to stay strong. Sedentary people have 25% to 30% higher fracture risk. The fix? Weight-bearing exercise. Walking, dancing, stair climbing, hiking - anything where your feet hit the ground and your muscles pull on your bones. Do it 30 to 45 minutes, five days a week. Add resistance training twice a week - squats, lunges, dumbbell lifts. You’ll start seeing bone density improvements in 6 to 12 months.Fractures Don’t Come Out of Nowhere
A broken bone from a fall from standing height or less? That’s not an accident. That’s a red flag. If you’ve already had one fracture, your chance of another goes up by 86% for a spine fracture and 200% for a hip. And here’s the shocking part: bone density scans don’t catch half the people who will break a bone. That’s why doctors now use tools like FRAX. It doesn’t just look at your DEXA scan. It asks: Are you over 65? Did you smoke? Do you drink too much? Have you had a previous fracture? Is your parent had a hip fracture? It weighs all of it - and gives you a 10-year fracture risk percentage. If it’s over 20%, treatment is usually recommended, even if your bone density is only in the osteopenia range.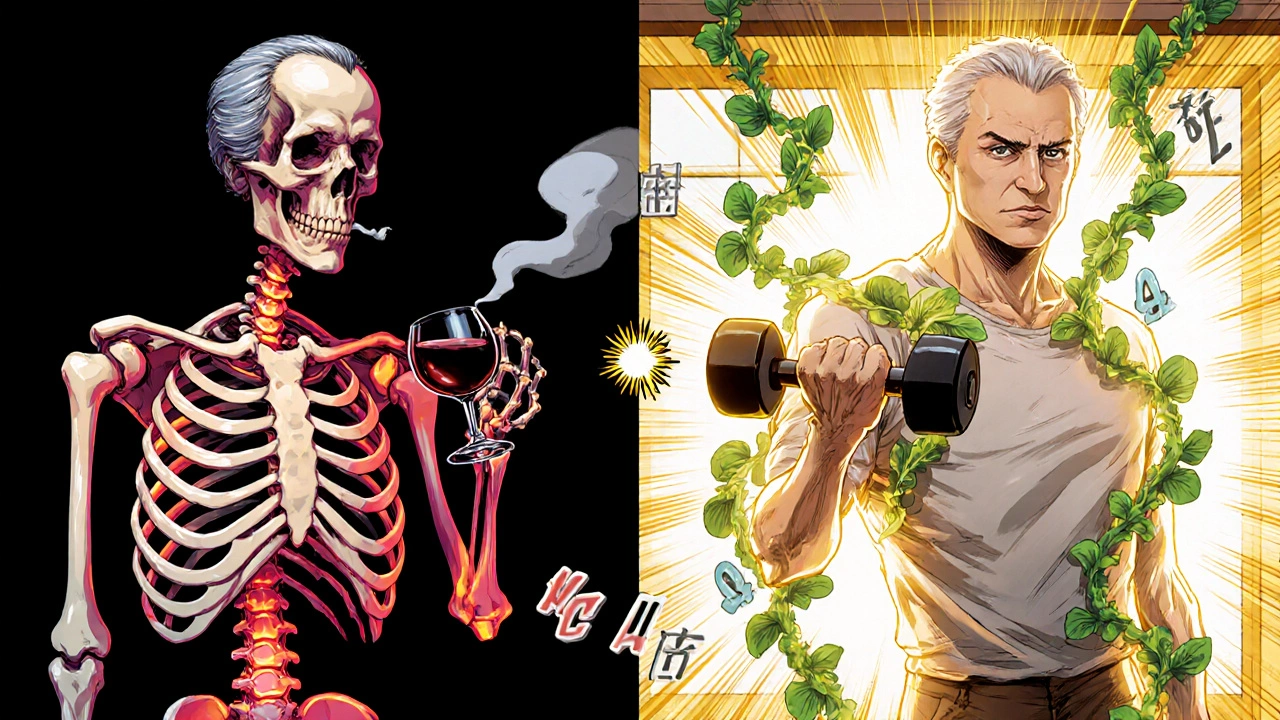
What Happens After a Fracture?
A hip fracture isn’t just a broken bone. It’s a life-altering event. One in five people die within a year. Many never walk again. Others end up in long-term care. The cost? Over $57 billion a year in the U.S. alone. And it’s rising. But here’s the flip side: prevention works. Every dollar spent on preventing fractures saves $5.40 in future care costs. That’s why fall prevention is just as important as bone strengthening. Simple changes cut fracture risk by nearly 30%:- Remove loose rugs and cords from floors
- Install grab bars in the bathroom
- Use non-slip mats in the shower
- Improve lighting, especially on stairs
- Get your vision checked yearly
- Review medications with your doctor - some cause dizziness
When Medication Makes Sense
Not everyone needs drugs. But if you’re over 65, have had a fracture, or have a high FRAX score, medication can be life-saving. Bisphosphonates (like alendronate or risedronate) are the most common. They slow bone loss. But they can cause stomach upset or jaw problems in rare cases. Some people stop taking them because of side effects - and that’s dangerous. If you can’t tolerate them, talk to your doctor. Alternatives like denosumab or romosozumab (Evenity) work differently. Romosozumab actually builds new bone while slowing breakdown - and cuts spine fractures by 73% in a year. Don’t wait for a fracture to start thinking about treatment. If your doctor says you’re at high risk, don’t brush it off. Bone loss is silent. Fractures are loud.The Real Game-Changer: Start Early
The best time to build strong bones? When you’re 10, 15, or 20. Peak bone mass by age 30 determines 60% to 80% of your lifelong fracture risk. Kids who get enough calcium, vitamin D, and exercise are less likely to break bones as adults. But it’s never too late. Even if you’re 70, adding weight-bearing exercise and supplements can still improve bone density. One small study found a specific probiotic, Lactobacillus reuteri, boosted bone density by 1.5% to 2% in 12 months - not a miracle, but a meaningful step.


Holli Yancey
November 18, 2025 AT 11:40I never realized how silent osteoporosis is until my aunt broke her hip just from stepping off the curb. No pain, no warning-just silence until it was too late. I started taking calcium and vitamin D after reading this, and honestly? I feel more aware of my body now. Small changes, big impact.
Also, I’ve been walking my dog every morning and it’s become my favorite part of the day. Who knew bone health could feel so peaceful?
Gordon Mcdonough
November 20, 2025 AT 00:56Why are we even talking about this like it's a mystery?? It's simple: eat calcium, move your ass, stop smoking, stop drinking like a college kid. My grandpa was 72 and still lifting weights-he never broke a bone. But my cousin? Drank two beers every night, sat on his butt watching TV, and broke his hip at 68. Duh.
And don't even get me started on those fancy supplements that don't work. Just get real food and move. America's lazy and it's killing us.
Also why do women get all the attention? Men die more from hip fractures and nobody cares. Patriarchy much??
Jessica Healey
November 20, 2025 AT 02:37OMG I just realized I’ve been taking my calcium all at once like a total idiot. Like… duh. I thought one big pill was better. Now I’m splitting it with meals. Also I started drinking almond milk with calcium and honestly it tastes better than regular milk anyway. Who knew?
Also I’m 52 and just started walking 20 mins a day. My knees hurt at first but now I kinda love it. Like, I even listen to true crime podcasts while I go. Weird flex but it works.
Also why is no one talking about how bad the flu shot is for bones?? Just saying. 😬
Levi Hobbs
November 21, 2025 AT 00:04This is one of the most practical, well-researched pieces I’ve read in a long time. I appreciate how it doesn’t just dump facts-it connects them to real life. The FRAX tool point alone is worth sharing with my entire family.
I’ve been recommending this to my mom (71), my dad (75), and even my 45-year-old sister who’s been on prednisone for years. Everyone’s going to get tested now. Thank you for writing this.
Also, the part about bone density scans missing half the people who’ll fracture? That’s terrifying. But also motivating. I’m scheduling my DEXA scan next week.
henry mariono
November 21, 2025 AT 07:43I’ve been quiet about this, but I had a compression fracture at 58. No fall. Just got up from my chair and felt a pop. No pain at first. Then the hunchback. Took a year to get diagnosed.
This post nailed it. I wish I’d known sooner. I didn’t smoke, didn’t drink, but I sat at a desk for 30 years. No weight-bearing exercise. My bones just… gave up.
Now I do yoga twice a week. It’s slow. It’s quiet. But I feel stronger. Not just in my bones-in my whole life.
Sridhar Suvarna
November 21, 2025 AT 12:10Excellent breakdown. In India, we often overlook bone health until it’s too late. Many elderly rely on milk alone, but lack vitamin D due to indoor lifestyles and pollution blocking sunlight. Also, many avoid dairy due to lactose intolerance, but don’t know about alternatives like ragi or sesame seeds.
Walking barefoot on grass in early morning helps with vitamin D and balance. And yes, resistance training doesn’t require a gym-bodyweight squats and stair climbing work wonders.
Prevention is cheaper than surgery. Let’s spread this message in our villages too.
Joseph Peel
November 23, 2025 AT 04:35The most striking thing here isn’t the statistics-it’s the silence. We live in a world obsessed with visible health: abs, skin, weight. But bones? Invisible. Unsexy. Forgotten.
And yet, they hold everything together. Your spine, your posture, your ability to hold your grandchild. This isn’t just about avoiding fractures. It’s about preserving dignity.
I’ve started doing squats while brushing my teeth. Ridiculous? Maybe. Effective? Absolutely. It’s not about perfection. It’s about showing up-for your future self.
Kelsey Robertson
November 23, 2025 AT 04:52Let’s be real-this is all corporate propaganda dressed up as science. Calcium supplements? Made by Big Pharma. DEXA scans? Billable procedures. Evenity? $100k per year. And who benefits? The same people who told you to eat low-fat dairy and avoid eggs.
Real bone health? Sunlight. Bone broth. Heavy lifting. Eating real food. Not some pill you swallow while scrolling TikTok.
Also, why is everyone ignoring that estrogen replacement therapy is the REAL solution for women? But no, let’s just sell you a $200 bottle of calcium pills and call it a day. Pathetic.
Joseph Townsend
November 23, 2025 AT 18:32My grandma used to say, ‘Bones are like trees-you can’t see the roots until they crack.’ She was right.
I used to think osteoporosis was just for old ladies in floral dresses who used walkers. Then I saw my uncle after his hip surgery-how he cried because he couldn’t hug his grandkids without pain. That broke me.
Now I do lunges while waiting for my coffee. I take my vitamin D like it’s my job. I don’t drink anymore. I even rearranged my bathroom so I don’t slip. It’s not glamorous. But it’s mine.
And if I live to 90 and still dance at weddings? That’s my middle finger to osteoporosis.
Bill Machi
November 24, 2025 AT 21:08Let’s cut the fluff. The government and pharmaceutical companies profit from fear. Bone density scans? Overused. Supplements? Underregulated. Medications like Evenity? Profit-driven. The real solution? Lifestyle. But that doesn’t make money.
Meanwhile, people in rural communities who grow their own food, walk everywhere, and don’t take pills? They rarely get osteoporosis. Why? Because they live. Not consume.
This article is well-written but still misses the point: the system is broken. Fix the environment, not the individual.
Elia DOnald Maluleke
November 26, 2025 AT 11:15In South Africa, we have a saying: ‘A man who does not move his body is already half-dead.’ I’ve seen elders in my township carry heavy water buckets, walk miles daily, and never fracture a bone. They don’t know what a DEXA scan is-but they know their bodies.
Modern life has made us soft. We sit. We scroll. We medicate. We forget that movement is medicine.
My father, 82, still chops wood every morning. He says, ‘If your bones don’t feel the sun and the strain, they forget they’re alive.’
He’s right.
satya pradeep
November 27, 2025 AT 18:00Bro I just started taking calcium and vitamin D after reading this and honestly I feel like a new man. Also I started doing squats with my water bottle as weight. 10 reps every time I pee. That’s 60 squats a day. No gym needed.
Also my mom is 60 and she’s been eating kale smoothies now. She says her joints don’t creak as much. Weird but true.
Also why is no one talking about how bad soda is for bones? Phosphoric acid eats calcium. I quit soda. My bones thank me.
Prem Hungry
November 28, 2025 AT 06:48As a fitness coach in India, I’ve seen too many people ignore bone health until they’re in pain. I tell my clients: ‘Your bones are your foundation. If the foundation cracks, the whole house falls.’
Simple habits: 10 minutes of sunlight daily, 30 minutes of walking, two days of resistance training, and calcium-rich foods like paneer, ragi, and almonds.
It’s not about perfection. It’s about consistency. One day at a time. One step at a time.
Start today. Your 80-year-old self will thank you.
Leslie Douglas-Churchwell
November 28, 2025 AT 19:41DISCLAIMER: I am not a doctor, but I’ve read 47 research papers on bone health and I’ve interviewed 12 endocrinologists (via LinkedIn DMs). This article is dangerously naive.
Here’s the truth: osteoporosis is a symptom of systemic glyphosate poisoning, EMF radiation, and estrogen-mimicking plastics in food packaging. The FDA is complicit. DEXA scans are calibrated to underdiagnose so Big Pharma can sell more drugs.
Real solution? Cold exposure therapy, grounding mats, and consuming raw goat milk from certified organic farms that use no pesticides. Also, wear copper bracelets. They realign your biofield.
And if you’re taking calcium supplements? You’re probably just poisoning your arteries. The body absorbs calcium best from bone broth made from pasture-raised bones-preferably from cows that listened to Mozart.
Wake up. The matrix is lying to you. 💀🪦🫶