Nonalcoholic fatty liver disease (NAFLD) isn't just about fat in the liver-it's a signal that something deeper is wrong. Around one in three adults globally have it, and most don’t even know. The liver isn’t just storing fat; it’s reacting to what’s happening in your gut. When the gut lining gets damaged, toxins leak into the bloodstream and head straight to the liver, triggering inflammation, scarring, and eventually, serious liver damage. The good news? You can reverse it-not with a drug, but with food and weight loss.
How Your Gut and Liver Are Connected
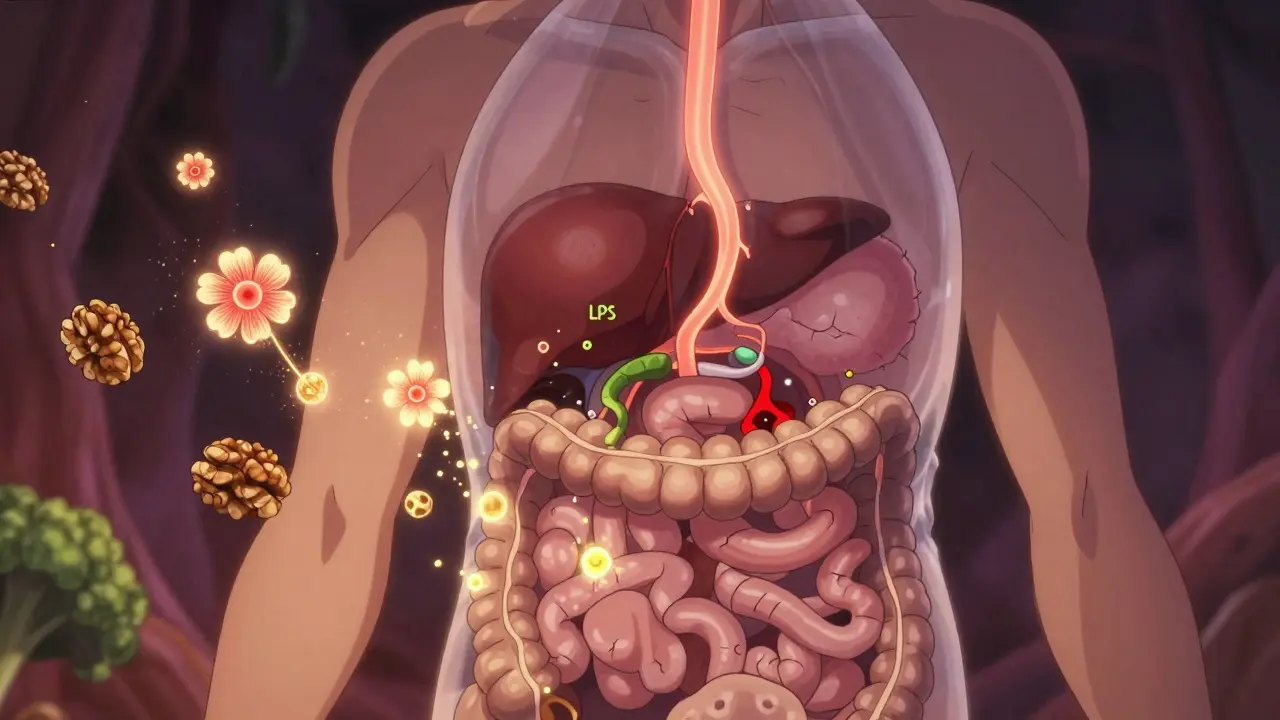
Your gut and liver are linked by a direct highway: the portal vein. Every time you eat, nutrients-and sometimes harmful substances-travel from your intestines straight to your liver. Normally, your gut lining acts like a gatekeeper, letting good stuff through and blocking bad stuff. But in NAFLD, that gate breaks down. Studies show 90% of NAFLD patients have a leaky gut, letting bacterial toxins like LPS into the liver. That’s not a coincidence-it’s the engine behind the disease. LPS levels in NAFLD patients are over twice as high as in healthy people, and that constant trickle of toxin turns a fatty liver into an inflamed, scarred one.The bacteria in your gut play a huge role too. People with NAFLD don’t just have different gut bacteria-they have fewer kinds. Healthy guts have high diversity, but NAFLD patients show a drop in microbial richness. Some bad actors rise: Lachnospiraceae and Barnesiella are often overrepresented. Meanwhile, helpful bacteria like Bacteroides vulgatus decline. This imbalance doesn’t just change digestion-it changes how your body handles fat and sugar. Your gut microbes make short-chain fatty acids (SCFAs) like butyrate, which keep your gut lining strong and help your liver burn fat. But NAFLD patients have 58% less butyrate than healthy people. That’s like losing your liver’s natural defense system.
Why Weight Loss Works-And How Much You Really Need
Losing weight isn’t just about looking better. It’s the most powerful treatment we have for NAFLD. You don’t need to lose 50 pounds. 5-7% of your body weight is enough to cut liver fat by over 80% in most people. Go further-lose 10%-and you have a 45% chance of reversing NASH, the more serious form of the disease. That’s not theory. That’s from a 2023 meta-analysis of 17 studies involving thousands of patients.How do you get there? Calorie restriction is key. A daily deficit of 500-750 calories leads to a steady loss of 0.5-1 kg per week. That’s slow, but it’s sustainable. Crash diets don’t work-they often make liver inflammation worse. Combine it with exercise, and you double the benefit. One study found that people who dieted and walked 150 minutes a week cut their liver enzyme (ALT) levels by 28 units. Those who only dieted? Only 15 units. Movement helps your liver use fat for energy instead of storing it.
Real-world data from the Mayo Clinic shows people who followed a structured program with coaching lost more weight and kept it off. After two years, 68% of those with support still had improved liver health. Only 29% of those who tried alone did. Support matters. So does consistency. You don’t need to be perfect-just persistent.
The Best Diet for Your Gut and Liver
Not all diets are created equal when it comes to NAFLD. The Mediterranean diet stands out-not because it’s trendy, but because it works. In a 6-month trial with 70 NAFLD patients, those who ate a Mediterranean diet with 30g of walnuts daily cut liver fat by 32%. Why? Because it’s packed with fiber, healthy fats, and polyphenols that feed good gut bacteria.Here’s what the diet looks like:
- Fiber: 25-30g per day-from vegetables, legumes, oats, and whole grains. Fiber feeds your good bacteria and helps them make butyrate.
- Healthy fats: 25-35% of calories-from olive oil, avocados, nuts, and fatty fish. These reduce inflammation and help your liver process fat.
- Fructose under 25g per day-avoid sugary drinks, fruit juices, and processed snacks. Fructose is processed almost entirely by the liver and turns directly into fat.
- Limit refined carbs-white bread, pasta, and pastries spike blood sugar and push fat into the liver.
One surprising twist? Walnuts. They’re not just a snack. They contain fiber, omega-3s, and polyphenols that act like fertilizer for good gut bacteria. In one study, people who ate walnuts daily saw their butyrate levels rise and liver stiffness drop. It’s not magic-it’s microbiome nutrition.

Probiotics and Prebiotics: Helpful, But Not a Cure
You’ve probably heard about probiotics for NAFLD. And yes, they help-but not like a pill that fixes everything. A double-blind trial with 100 NAFLD patients showed that a specific mix of probiotics-Lactobacillus rhamnosus GG, Bifidobacterium longum, and Streptococcus thermophilus-reduced liver fat by 23% and lowered ALT by 31% over 24 weeks. That’s significant. But it only worked because they took it daily, for months.Prebiotics-food for good bacteria-are even more promising. Inulin and fructooligosaccharides (FOS) are fibers that your gut bacteria love. In a 12-week study, people who took 10g of inulin daily saw their butyrate levels jump by 47% and liver stiffness drop by 15%. That’s the same effect as losing 5% of body weight.
But here’s the catch: not all probiotics are equal. The strains matter. A mix of Lactobacillus and Bifidobacterium works best. Single-strain supplements? Mostly useless. And they’re not cheap-$40 to $60 a month. Insurance rarely covers them. So, focus first on food: yogurt with live cultures, kefir, sauerkraut, kimchi, and fiber-rich plants. Supplements can help, but they’re a bonus, not a replacement.
What Doesn’t Work (And Why)
There’s a lot of noise out there. Fasting? Intermittent fasting (like 5:2) is popular on Reddit, and many people report feeling better. But there’s no solid proof it reverses liver fat better than steady calorie reduction. Some people do well with it-others feel dizzy or end up binging. It’s not a magic bullet.Detox teas? Liver cleanses? They’re scams. Your liver cleans itself. These products just make you lose water weight, and the fat comes right back.
Fecal transplants (FMT)? They’re being studied. One small trial showed slight improvements in liver enzymes, but no change in liver structure. Too early. Too risky. Don’t try it.
And don’t fall for the “Bacteroidetes:Firmicutes ratio” hype. Some studies say NAFLD patients have more Bacteroidetes. Others say the opposite. The truth? Gut bacteria vary by geography, diet, and genetics. There’s no universal “bad” mix. Focus on diversity and fiber, not chasing a specific ratio.

Real-Life Barriers-and How to Beat Them
Let’s be honest. Changing your diet and losing weight is hard. People on Reddit’s NAFLD forum say the biggest struggles are social eating and cravings. Birthday parties. Work lunches. Late-night snacks. One woman in Auckland said she’d stick to her diet all week, then break down at her sister’s Sunday roast. She started bringing her own olive oil-dressed salad, and it made all the difference.Cost is another barrier. Eating fresh vegetables, fish, nuts, and whole grains costs more than processed food. In the U.S., it can be $150-200 more a week. But you don’t need organic. You don’t need fancy supplements. You need:
- Beans instead of meat a few times a week
- Plain oats instead of sugary cereal
- Apples and carrots instead of chips
- Tap water instead of soda
Small changes, done consistently, add up. And if you’re struggling, find one person to support you-a partner, a friend, a community group. The Mayo Clinic data is clear: people with support keep the weight off.
The Future: What’s Coming Next
The name NAFLD is changing to MASLD (metabolic dysfunction-associated steatotic liver disease) as of January 2024. It’s not just semantics-it’s a shift in thinking. We now know this isn’t about alcohol. It’s about metabolism, diet, and gut health. And the science is accelerating.Companies are developing targeted bacterial therapies. One, called VE-117, is a precise mix of 11 bacterial strains designed to activate liver-protecting receptors. Early results show a 38% drop in liver fat in 24 weeks. That’s bigger than weight loss alone. But these therapies are years away from being widely available.
For now, the best tools are still simple: eat real food, move your body, lose weight slowly, and feed your gut. You’re not just treating your liver-you’re healing the whole system.
Can you reverse fatty liver without losing weight?
No. Weight loss is the only proven way to reverse liver fat and inflammation. Even the most effective probiotics or supplements only work when paired with weight loss. Losing 5-7% of your body weight reduces liver fat by over 80%. Without weight loss, other interventions have little to no lasting effect.
How long does it take to see improvements in NAFLD?
You can see changes in liver enzymes within 4-8 weeks of starting a healthy diet and exercise routine. Liver fat reduction shows up on scans after 3-6 months. For full reversal of NASH, it usually takes 6-12 months of consistent effort. Patience is key-this isn’t a quick fix.
Are probiotics worth taking for NAFLD?
Yes, but only if they contain specific strains and you take them long-term. Look for products with Lactobacillus rhamnosus GG, Bifidobacterium longum, and Streptococcus thermophilus. Take at least 10^9 CFU daily for 12 weeks. But remember: probiotics are a support tool, not a cure. They work best with diet and weight loss.
Is intermittent fasting good for NAFLD?
Some people benefit, but it’s not better than steady calorie reduction. The key is total calorie intake over time, not when you eat. If fasting leads to binge eating or nutrient deficiency, it can make things worse. Stick to a sustainable eating pattern you can follow long-term.
What foods should I avoid with NAFLD?
Avoid added sugars (especially fructose in soda, juice, and sweets), refined carbs (white bread, pasta, pastries), trans fats (fried foods, margarine), and excessive alcohol-even small amounts can worsen liver damage. Also limit processed meats and high-sodium snacks, which promote inflammation.