If you spend even a few minutes browsing through TV commercials or scrolling on health forums, you’ll notice Lipitor’s name pops up a lot. For a good reason—it’s been the world’s best-selling prescription drug for years. Still, there’s this odd gap: so many people take it, but not everyone understands exactly what it does, how it works in your body, or why doctors seem to hand out statins like Halloween candy. Want the real story, backed by facts, no technical mumbo-jumbo or wild internet rumors? You're in the right place.
What Exactly Is Lipitor and How Does It Work?
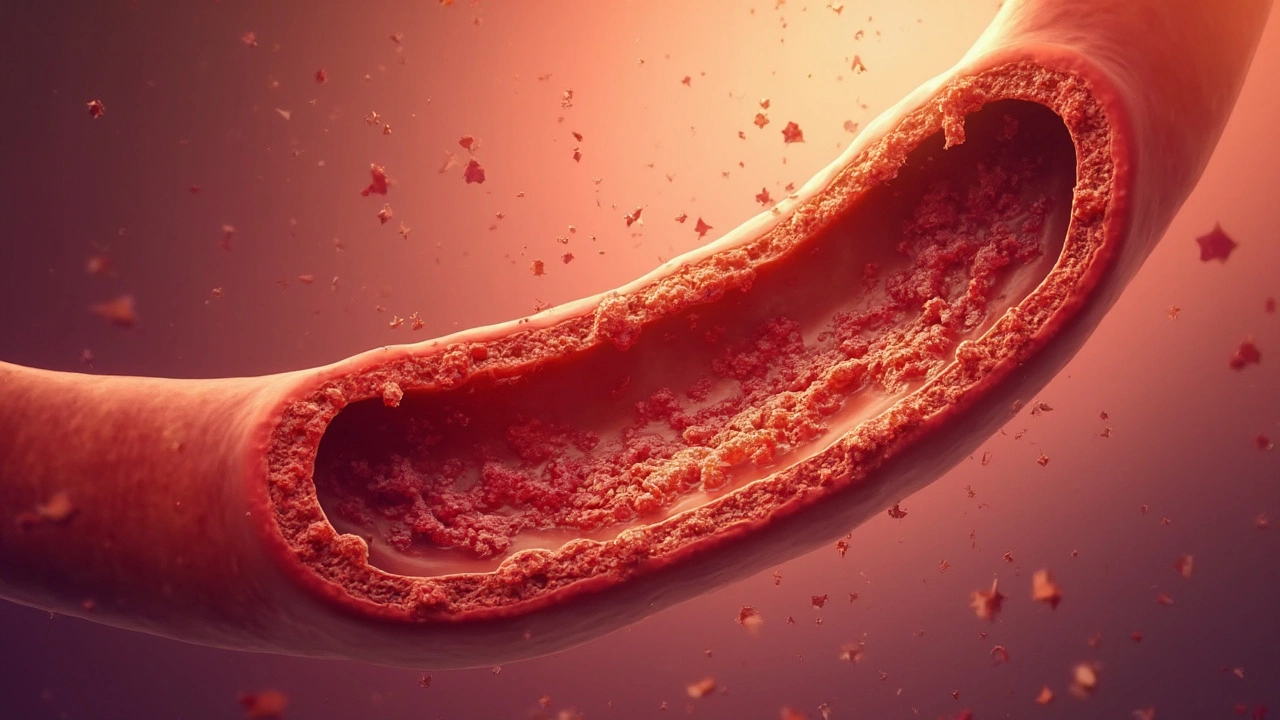
Lipitor, known by its generic name atorvastatin, is a statin—a group of drugs tuned to cut cholesterol. It’s not just about numbers on a lab sheet; the real goal is keeping your arteries from getting clogged with fatty deposits, which can lead to a heart attack or stroke. Lipitor works by blocking HMG-CoA reductase, a liver enzyme that’s a key player in making cholesterol. This slows down new cholesterol production and gives your liver more time to grab extra cholesterol from your bloodstream and break it down.
The story doesn’t stop with just lower cholesterol. Lipitor specifically targets LDL—think of it as the “bad” cholesterol that likes to stick to your artery walls. It also nudges up your HDL, or “good” cholesterol, which helps carry cholesterol away from blood vessels for safer disposal. Studies from places like the New England Journal of Medicine have shown that reducing LDL with statins can shrink heart attack risk by as much as 30% in people already at risk. That’s why Lipitor found its way to so many medicine cabinets after it hit the market in 1997.
Now, here’s the twist—Lipitor doesn’t work the same for everyone. Some people see their numbers drop like a rock. Others might need a stronger dose or extra help, maybe even another cholesterol medicine if their bodies just don’t respond. Genes, diet, and even your gut bacteria play a role in how well you respond. So, if you’re comparing results with someone else, remember it’s not a one-size-fits-all deal.
Lipitor isn’t just about cholesterol, either. Recent studies show it may help lower inflammation markers like CRP, an emerging sign of hidden artery problems. Researchers in the last decade have linked statins to a drop in hospital visits from unstable heart disease and possibly lower risk of certain strokes. But nothing is magic—if you’re pounding burgers and skipping your walks, no pill can undo all the damage. Lifestyle and medicine are best friends here.
Who Should (and Shouldn’t) Take Lipitor?
The first thing to clear up: Lipitor isn’t just for the elderly or people who’ve already had a heart attack. Doctors often suggest it if your LDL cholesterol is too high—usually above 130 mg/dL if you are at risk, or 190 mg/dL no matter what. You might also get handed a statin prescription if you have diabetes, existing heart disease, or even lots of risk factors—like high blood pressure and family history—that stack the odds against your arteries.
The U.S. Preventive Services Task Force released fresh guidelines in 2022. They recommend statins for adults ages 40–75 who have one or more heart disease risk factors and at least a 10% chance of having a cardiovascular event in the next 10 years. Here’s where it gets interesting: more than half of Americans over 40 actually hit that definition. But not everyone needs the same amount or even the same drug. It’s all about your personal dance with risk versus benefit.
Of course, not everyone is a good candidate. Lipitor isn’t friendly to pregnant women or anyone with active liver disease. If you’ve had unexplained muscle pains or very high liver enzymes from prior statin use, bring it up with your doctor. Also, rare genetic conditions like familial hypercholesterolemia sometimes need far more aggressive treatment plans. People with these conditions can have LDL levels that could make any statin sweat.
Ever wonder what the numbers actually look like? Here’s a quick breakdown:
| Category | Lipitor Dose (mg) | Average LDL Reduction (%) |
|---|---|---|
| Low risk | 10 | Approximately 39% |
| Moderate risk | 20 | Approximately 43% |
| High risk / Aggressive goals | 40-80 | Up to 60% |
That table shows why some folks start low and others ramp up—your dose isn’t just random, it’s matched to your risk, goals, and sometimes how your liver and muscles handle the medicine. People with a family history of bad reactions, or who are already taking lots of different meds, might need more check-ins. Combination therapy (pairing Lipitor with medicines like ezetimibe or PCSK9 inhibitors) sometimes adds extra punch—but only if your cholesterol needs serious muscle.
Real-World Benefits Backed by Data
Let’s ditch the hype and get into the hard numbers. Lipitor has been around for almost three decades, and there’s a mountain of studies on its benefits. The most famous was the TNT Study (Treating to New Targets), where thousands of patients with heart disease took either 10 mg or 80 mg of Lipitor daily. Over nearly 5 years, those on the higher dose had about a 22% lower chance of major cardiovascular events—like heart attack or stroke—compared to the low-dose group.
It’s not just about big, obvious heart attacks. Lipitor and other statins have cut down on hospital visits for chest pain, reduced the need for stents, and even dropped mortality rates in patients with diabetes or kidney issues. There’s good evidence from trials like ASCOT and SPARCL showing protection against certain kinds of stroke. Doctors have noticed that patients on statins, especially those who stay on them consistently, don’t bounce back to the hospital as often.
Want a fun fact? Back before the patent ran out in 2011, Lipitor made more than $125 billion for Pfizer, its original maker. That wasn’t just clever marketing—prescription rates rocketed because so many studies proved real, repeatable patient benefits across diverse groups and backgrounds.
Another interesting twist: new research hints that statins, including Lipitor, may help reduce inflammation in your blood vessels, slowing down the process that makes plaques unstable. Less inflammation means a lower chance of sudden, dangerous blockages. That may be why some doctors stick with their statin prescriptions, even when cholesterol numbers look good—because there’s more to heart health than just LDL.
Common Side Effects, Myths, and How to Manage Them
This is where most people get nervous. Type “Lipitor side effects” into Google and you’ll find everything from “I felt great” to “my muscles turned to jelly.” The most common complaints are headaches, mild stomach upset, and muscle aches. Studies say only about 5–10% of people actually get muscle-related symptoms, but the risk does go up with higher doses and certain combinations of drugs or supplements—like grapefruit juice, which is famous for messing with statin metabolism.
There’s a lot of confusion out there about muscle pain. Most of the time, if you feel mild aches that go away when you take a break from the medicine, it’s rarely dangerous. But if you get dark urine, severe weakness, or pain that just won’t quit, call your doctor fast—those can be red flags for serious, thankfully very rare, problems like rhabdomyolysis (a kind of muscle breakdown). For most people, switching brands, lowering the dose, or spacing Lipitor away from other meds fixes the issue. Hydration and regular exercise also seem to help muscle tolerance in people who are otherwise healthy.
A few other side effects pop up in a tiny minority—liver enzyme bumps (usually not dangerous), slight increases in blood sugar (mainly in folks pre-diabetic anyway), and sometimes memory fog. The best tip? Check your liver enzymes before starting and again around 6-12 weeks after, then relax unless you feel truly off. Most people see the enzyme numbers settle with time.
Let’s explode a big myth: Statins like Lipitor don’t melt your muscles, erase your memory, or make you live in fear. The vast majority handle Lipitor with no problem, especially with regular doctor check-ins and honest reporting of symptoms. People who are worried about diabetes risk should remember: the heart benefits almost always outweigh the slight uptick in blood sugar—but it’s smart to track your numbers if you’re already borderline diabetic.
- Space out Lipitor away from grapefruit juice.
- Take it at the same time daily (evening works best for most people—cholesterol peaks then).
- Stay active: regular exercise makes you less likely to notice side effects.
- Honest talk with your doctor always trumps searching for horror stories online.

Tips for Getting the Most from Lipitor (Without Losing Your Mind Over It)
If you’re new to Lipitor or thinking about it, you might feel anxious about keeping things simple—and safe. First, make your pharmacist your ally. They’ll spot nasty drug combos and remind you to keep the pill out of blazing heat or direct sunlight (Lipitor hates both). Next, consistency is your friend. Set an alarm if, like me, you forget things easily. If you accidentally skip a dose, don’t double up the next day—just get back on track.
Look at Lipitor like your health insurance: it’ll have your back in a crisis, but you’re still in control of the day-to-day. If your doctor is monitoring you, expect a cholesterol test about 6–12 weeks after you start, then at least once a year if all goes well. That’s how they catch side effects or spot hidden problems before they get big. Jot down any muscle aches or weird symptoms in your phone—honestly, phones make the best memory aids.
Get serious about lifestyle, too. No prescription can do it alone. More veggies and fiber, cutting back on saturated fats, ditching tobacco, and maybe adding a fish oil capsule can make your statin work even harder. Real-world data from big cholesterol clinics shows people who tweak their diet see better results, sometimes even enough that their meds go down after a while. Success really is a team effort between you, your medicine, and your kitchen.
If price is an issue, know that generic atorvastatin works every bit as well. Most insurance plans cover it, and it often costs less than a fast-food meal per month if you use discount cards. If you’re worried about long-term use, there’s good news: most people don’t see any extra side effects, even after 10 years or more. It’s tested, trusted, and straightforward—as long as you keep the people who prescribe it in the loop about any new stuff in your health story.
End of the day, Lipitor is more than a cholesterol fixer; it’s a real shot at dodging serious trouble with your heart or brain, especially if you know exactly what you’re taking, why, and how to do it right. Most people thrive on it, and if you don’t, there’s almost always a Plan B. Stay curious, stay honest with your healthcare team, and remember—one pill doesn’t own your story, but it can make the journey a lot smoother.


Jimmy Gammell
July 18, 2025 AT 16:00Hey folks, this post about Lipitor is really helpful! :) I've seen lots of people confused about cholesterol meds. It's good to know exactly how atorvastatin works and what to watch out for.
One thing I always recommend is checking with your doc regularly when you're on Lipitor, especially cause side effects can sneak up. Staying informed and proactive totally helps keep things safe, you know?
Also, anyone else here found any good lifestyle tips that helped alongside this medication? I think combining diet and exercise with meds is super key.
Ellie Haynal
July 18, 2025 AT 16:46Honestly, I can’t stress enough how important it is to be cautious with Lipitor and stuff like that. So many doctors just hand out prescriptions without explaining the potential nightmares you could face. I’ve seen people just ignore side effects until it’s too late.
This post is a wake-up call! If you don’t advocate for your health, who will? Like, seriously, sometimes the medical system acts like it’s only about stats and not people. This drug is powerful, but that means respecting it and monitoring your body closely.
And for anyone thinking they can just take it recklessly—I’ve got news for you. It’s not worth putting your liver or muscles at risk. Better to be informed than sorry!
fred warner
July 18, 2025 AT 18:10Great post! The benefits of Lipitor really can't be overstated for those at risk of cardiovascular issues. It's impressive how atorvastatin can lower LDL cholesterol so effectively.
That said, adhering to your prescribed dose and lifestyle adjustments is essential to maximize the benefits and minimize side effects. It's a partnership with your healthcare provider.
I've been recommending that people keep an eye out for common side effects like muscle pain and fatigue, and report them promptly. Early detection can prevent more serious complications.
Overall, the safety profile of Lipitor is solid when used appropriately. It offers hope for many who need it.
Veronica Mayfair
July 18, 2025 AT 19:33Omg, yes!! This post is just so informative 😍 I love how it breaks down the facts to avoid confusion. Cholesterol is such a big deal but sometimes scary 😅
Have any of you tried combining Lipitor with some natural supplements or foods? I heard about people taking omega-3s alongside their meds. Does anyone know if that’s safe?
Also, vibes to everyone on their health journey! Sending good energy your way 💖✨
Nicholas Blackburn
July 18, 2025 AT 20:56Alright, let me get real here. People often overlook the ugly truths behind these so-called miracle drugs. Lipitor might 'lower cholesterol' but what about the long-term consequences they conveniently don't talk about? This isn't some magic pill that fixes everything without a cost.
Anyone naive enough to think otherwise is just inviting trouble. You’d better watch yourself carefully, research deeply, and question everything your doctor says because the pharmaceutical industry thrives on your ignorance.
It’s high time we stop glorifying these drugs blindly and start demanding transparency!
Anthony Coppedge
July 18, 2025 AT 22:20This article does a solid job explaining how to use Lipitor safely. One thing I always emphasize with patients is understanding the importance of timing your dose—taking it at night usually works best because cholesterol production peaks then.
Also, never hesitate to inform your healthcare provider of muscle pain or weakness, as these can be signs of serious side effects. It’s critical to balance benefits with caution.
Remember, medication is just one part of comprehensive cholesterol management including diet and regular exercise.
Stay informed and stay safe, everyone!
Joshua Logronio
July 18, 2025 AT 23:43Yo, anyone else think the whole Lipitor craze has some underground agenda? I mean, why push this stuff so hard when lifestyle changes should come first? Feels like big pharma is making billions off us being lazy.
Not saying the drug doesn’t work but I always wonder what they’re not telling us. Side effects and who really benefits—hmmmmm 🤔
Stay woke, folks. Don’t just blindly swallow a pill, read up and question everything.
Rahul Kr
July 19, 2025 AT 01:06Thanks for sharing this post! It's important to have balanced info on Lipitor because fear and misinformation can lead people to avoid beneficial treatments.
While being watchful about side effects is sensible, most users tolerate Lipitor well when monitored. Complementing medication with a healthy diet definitely enhances outcomes.
And it’s great to remember that everyone responds differently, so open communication with your doctor is key.
Good luck to all navigating their health journeys! 😊
Dave Barnes
July 19, 2025 AT 03:53Philosophically speaking, the discourse around Lipitor epitomizes modern society’s tension between technology's promises and human vulnerabilities. Here lies a complex medicine reconciling the fragility of our biochemistry against the looming threats of cardiovascular disease.
While the drug operates at a molecular scale, its impacts ripple through lives and ethical discussions. What does safe use mean in a world constantly negotiating risks?
Deep contemplation on the integration of such therapies invites both awe and caution.
Kai Röder
July 25, 2025 AT 01:33This post offers a comprehensive overview but I think it’s prudent to underscore the necessity of personalized medical advice. Clinical guidelines serve as frameworks but each patient’s context matters greatly.
Effective communication with clinicians ensures therapeutic decisions that balance efficacy and safety properly. Lipitor can be tremendously beneficial, yet it mandates respect for individual nuances.
Collective awareness and scholarly discussion around such medications further enhance public health literacy.
Brandi Thompson
August 1, 2025 AT 00:13Seriously, the whole Lipitor thing? It's like people don’t want to hear the harsh realities. This drug messes with your body in ways you won't notice until it's too late. The article sounds all shiny and safe, but trust me, I've read too many horror stories to buy that fully.
And don't get me started on how some patients get brushed off when they report side effects. It's like discomfort and pain don't matter in the grand scheme of cholesterol numbers.
If you're thinking about taking Lipitor, just be prepared: hoops to jump through, side effects that may ruin your day, and doctors who sometimes don't listen.
Stay alert and keep pushing for real answers!