When your body doesn’t make enough parathyroid hormone, your calcium drops-and that’s not something you can ignore. Hypoparathyroidism isn’t just a lab result. It’s numb lips, muscle cramps, fatigue that won’t quit, and the constant fear of your next calcium crash. For most people, this condition happens after thyroid or neck surgery, but it can also come from genetics, autoimmune issues, or radiation. The goal isn’t just to raise calcium. It’s to keep it steady, avoid kidney damage, and actually feel like yourself again.
Why Calcium and Vitamin D Alone Aren’t Enough
You might think, "Just take more calcium and vitamin D," but that’s where things get tricky. In hypoparathyroidism, your body can’t convert regular vitamin D into its active form because parathyroid hormone (PTH) is missing. That’s why you need active vitamin D-like calcitriol or alfacalcidol-not plain vitamin D3. Calcitriol works 2.3 times faster than regular vitamin D supplements, according to the 2018 REPLACE trial. Without it, your body can’t absorb calcium from food or pull it from your bones, no matter how much you take.
Calcium supplements are necessary, but not all are created equal. Calcium carbonate is the go-to because it’s 40% elemental calcium. That means you need less of it. For example, 1,250 mg of calcium carbonate gives you 500 mg of actual calcium. Calcium citrate? Only 21% elemental calcium. You’d need to swallow way more pills to get the same dose. And you have to take it with meals-not just for absorption, but because it helps bind excess phosphate in your gut. Too much phosphate? That’s a problem too. It pulls calcium out of your blood and can wreck your kidneys.
Dosing: The Tightrope Walk
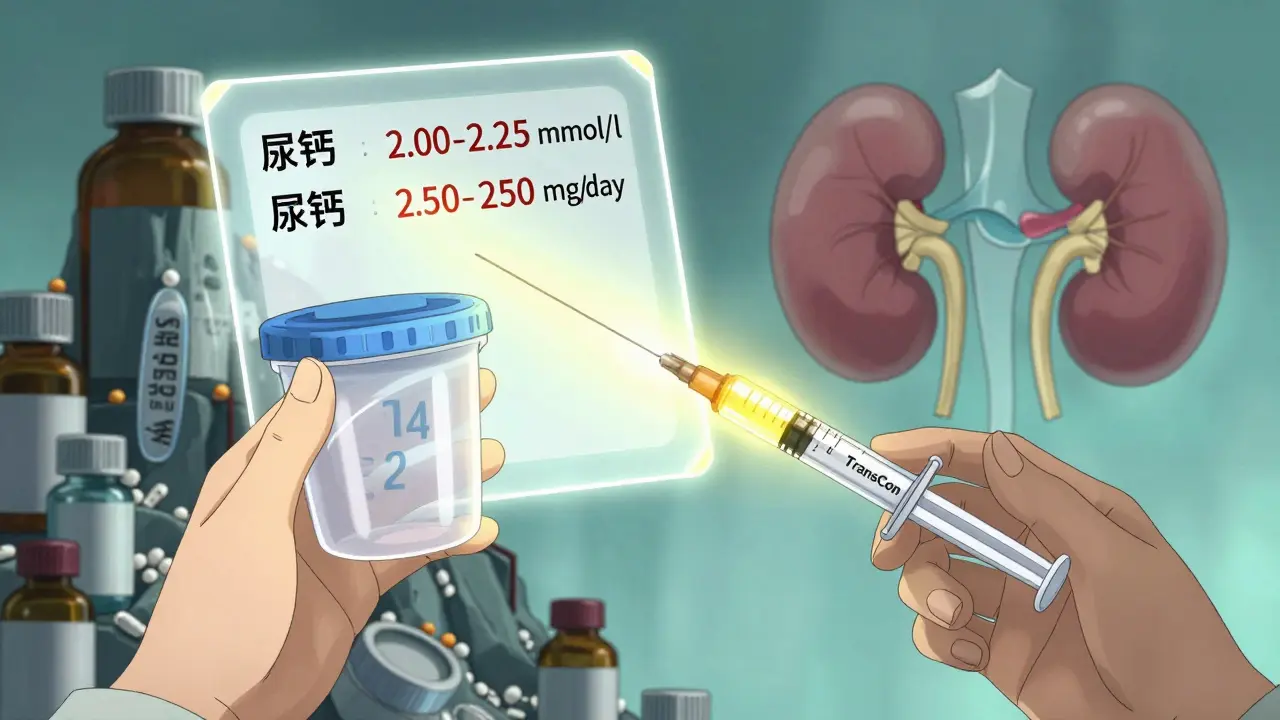
Most people start with 1,000 to 2,000 mg of calcium per day, split into two or three doses. Some need more. But here’s the catch: if you go too high, you start peeing out too much calcium. That’s called hypercalciuria. And that’s how kidney stones form. The target? Keep your serum calcium between 2.00 and 2.25 mmol/L (8.0-8.5 mg/dL). Not normal. Not high. Just below the middle of the normal range. That’s the sweet spot, according to Parathyroid UK and the Mayo Clinic.
Active vitamin D usually starts at 0.25 to 0.5 mcg daily. Too little? You’ll still feel numb and tired. Too much? You risk calcium buildup in soft tissues-your heart, lungs, even your brain. The Cleveland Clinic found that patients with calcium levels above 2.35 mmol/L for over 15 years had nearly three times the risk of brain calcification. That’s not theoretical. It shows up on MRIs.
And don’t forget magnesium. If your magnesium is below 1.7 mg/dL, your body can’t respond to PTH-even if you replace it. Magnesium deficiency is common in hypoparathyroidism. Supplement with 400-800 mg of magnesium oxide or 200-400 mg of magnesium citrate daily. It’s simple. It’s cheap. And it makes a difference.
What You Should Eat (and Avoid)
Diet matters more than most doctors admit. You need calcium-rich foods: dairy (300 mg per serving), kale (100 mg per cup), broccoli (43 mg per cup). But you also have to cut back on phosphate. That means saying no to soda (500 mg per liter), processed meats (150-300 mg per serving), and hard cheeses (500 mg per ounce). A single slice of cheddar can put you over your daily limit.
Most guidelines recommend keeping phosphate intake under 1,000 mg per day. That’s not easy when so much of what we eat is processed. Reading labels helps. Look for "phosphoric acid," "calcium phosphate," or anything with "-phos" in it. These aren’t natural. They’re additives. And they’re sneaky.
Some patients try phosphate binders, but the evidence is mixed. Calcium supplements already act as binders when taken with meals. Adding more binders might mean even more pills-and more risk of constipation or worse. Stick to food first. Then adjust meds if needed.
When the Standard Treatment Fails
One in three people still struggle, even with perfect dosing. They need more than 2 grams of calcium or more than 2 mcg of active vitamin D daily. They still have high urine calcium. They’re still tired, anxious, or getting kidney stones. That’s when you need to think beyond pills.
Recombinant PTH (like Natpara or Forteo) is an option. It’s not a cure. It’s a replacement. You inject it once a day. It brings calcium levels down to normal without needing huge doses of supplements. Studies show it cuts calcium and vitamin D needs by 30-40%. But it’s expensive-around $15,000 a month. And it’s not easy to get. Insurance often requires 30-45 days of paperwork. Many patients give up.
There’s hope on the horizon. TransCon PTH, a long-acting PTH prodrug, showed in a 2022 trial that 89% of patients normalized their calcium with just one daily injection. No more multiple pills. No more constant monitoring. Just one shot. It’s not approved yet, but it’s coming. Trials are wrapping up. Approval could happen by late 2026.
Monitoring: What to Check and How Often
You can’t manage what you don’t measure. Every 1-3 months, you need:
- Serum calcium (target: 2.00-2.25 mmol/L)
- Serum phosphate (target: 2.5-4.5 mg/dL)
- Serum magnesium (target: 1.7-2.2 mg/dL)
- 24-hour urinary calcium (target: under 250 mg/day)
And don’t skip the urine test. It’s the only way to catch hypercalciuria before it damages your kidneys. The 2017 HypoPT Natural History Study found that 35-40% of patients on standard therapy develop high urine calcium-and their risk of kidney stones jumps 5-7 times. That’s not rare. That’s predictable. And preventable.
Once you’re stable, annual checks are fine. But if you’re new to treatment or adjusting doses, check every month. Your body is sensitive. Small changes in timing, food, or stress can throw you off.

Living With It: The Real Challenges
A 2021 survey of 412 patients found that 68% struggle to keep calcium stable. 52% have symptoms every day. They call it the "calcium rollercoaster"-one day numb fingers, the next day bone-deep fatigue. Many take six to ten pills a day. Constipation from calcium? Common. Nausea from vitamin D? Not rare.
Some find relief with split-dose calcium: four or five smaller doses spread through the day instead of two or three big ones. It smooths out the highs and lows. Others swear by taking vitamin D at bedtime. It’s absorbed better when your body isn’t digesting food.
And don’t underestimate the mental load. Constantly checking food labels. Worrying about kidney function. Fear of a sudden drop. It’s exhausting. That’s why education matters. Know the early signs: tingling around the mouth, cramping in hands or feet, anxiety, heart palpitations. Keep calcium tablets with you. Chew two or three if you feel a crash coming. It buys you time until you can get help.
Who Should Manage Your Care?
Start with an endocrinologist. You need someone who’s seen this before. In the first three months, expect 3-4 visits. Once stable, you can switch to annual visits. But here’s the problem: 78% of family doctors say they don’t feel trained to manage hypoparathyroidism. So if your primary care provider doesn’t know what to do, don’t push back. Ask for a referral. You deserve expertise.
And if you’re struggling-really struggling-don’t wait. If you need more than 2 grams of calcium or 2 mcg of vitamin D daily, or if you’re still having symptoms, ask about PTH replacement. It’s not a last resort. It’s a tool. And it might be the key to your quality of life.
The Big Picture: Balance Over Perfection
Hypoparathyroidism isn’t about normalizing numbers. It’s about living without symptoms. It’s about protecting your kidneys. It’s about not needing ten pills a day. The best treatment is the one that works for you-not the one that looks good on paper.
There’s no perfect formula. Some people do fine with pills. Others need injections. Some need to change their diet. Others need magnesium. The goal isn’t perfection. It’s stability. And if you’re not there yet, you’re not alone. New treatments are coming. And you have more options than you think.
Can I manage hypoparathyroidism with just vitamin D3 and calcium supplements?
Yes, for many people. But only if you use active vitamin D (calcitriol or alfacalcidol), not regular vitamin D3. Plain D3 won’t work because your body can’t activate it without parathyroid hormone. Calcium supplements must be taken with meals to help control phosphate and improve absorption. Most people need 1,000-2,000 mg of calcium daily in divided doses, along with 0.25-0.5 mcg of active vitamin D. Still, about 25-30% of patients can’t stabilize their levels this way and need PTH replacement.
Why is my urine calcium high even though my blood calcium is normal?
High urine calcium means your kidneys are filtering out too much calcium, even if your blood levels look okay. This often happens when you’re taking too much calcium or vitamin D. It’s a warning sign. Over time, it can lead to kidney stones or even kidney damage. The fix isn’t to lower blood calcium-it’s to reduce total calcium intake, cut back on sodium, and sometimes add a thiazide diuretic like hydrochlorothiazide. Always check your 24-hour urine calcium before increasing doses.
Do I need to avoid all dairy if I have hypoparathyroidism?
No. Dairy is actually a great source of calcium. One cup of milk has about 300 mg. The issue isn’t dairy-it’s high-phosphate foods. Hard cheeses, processed meats, and soda are the real problems. You can and should include dairy in your diet. Just avoid processed versions like processed cheese or flavored yogurts that have added phosphates. Stick to plain milk, yogurt, and soft cheeses.
Is magnesium really that important for hypoparathyroidism?
Yes. Low magnesium blocks your body’s ability to use PTH-even if you’re taking PTH replacement. About 20% of hypoparathyroid patients have low magnesium without knowing it. Symptoms include muscle cramps, fatigue, and irregular heartbeat. If your magnesium is below 1.7 mg/dL, supplement with 400-800 mg of magnesium oxide or 200-400 mg of magnesium citrate daily. Many patients see fewer symptoms within weeks.
What’s the difference between Natpara and Forteo?
Both are forms of PTH replacement, but they’re different. Natpara is recombinant human PTH(1-84), made to fully replace the hormone your body lacks. Forteo (teriparatide) is PTH(1-34), a shorter piece of the hormone, originally designed for osteoporosis. Natpara is approved specifically for hypoparathyroidism. Forteo is used off-label. Natpara is more effective at normalizing calcium without high-dose supplements, but it’s harder to get due to strict prescribing rules. Forteo is cheaper and more widely available but may not control phosphate as well.
Can I ever stop taking calcium and vitamin D for hypoparathyroidism?
Almost never. Hypoparathyroidism is usually permanent. Even if it starts after surgery, the parathyroid glands rarely recover fully. Some people with temporary cases (like after thyroid surgery) might taper off after 6-12 months if labs normalize-but that’s rare. Most need lifelong treatment. The goal is to find the lowest effective dose that keeps you symptom-free and protects your kidneys.
Are there new treatments coming for hypoparathyroidism?
Yes. TransCon PTH, a once-daily injectable long-acting PTH, showed in a 2022 trial that 89% of patients normalized their calcium levels with just one shot. It’s designed to reduce pill burden and improve stability. Approval is expected by late 2026. Gene therapies targeting the calcium-sensing receptor are in early research, but human trials won’t start until after 2026. For now, PTH replacement is the biggest advance in decades.
If you’re managing hypoparathyroidism, you’re not just treating numbers-you’re fighting for stability, comfort, and control. The path isn’t easy, but it’s clear: know your numbers, stick to the basics, ask for help when you need it, and keep an eye on what’s next. You’re not alone in this.