Getting a medication dose wrong isn’t just a mistake-it can kill someone. In 2022, over 1,200 reported incidents of incorrect dose changes led to nearly 300 cases of patient harm, according to the ECRI Institute. Most of these weren’t caused by reckless staff. They happened because of broken communication, rushed handoffs, or verification systems that felt like busywork. The truth is, dose verification isn’t about checking boxes. It’s about building layers of protection that actually work when it matters.
Why Dose Changes Are the Most Dangerous Moment
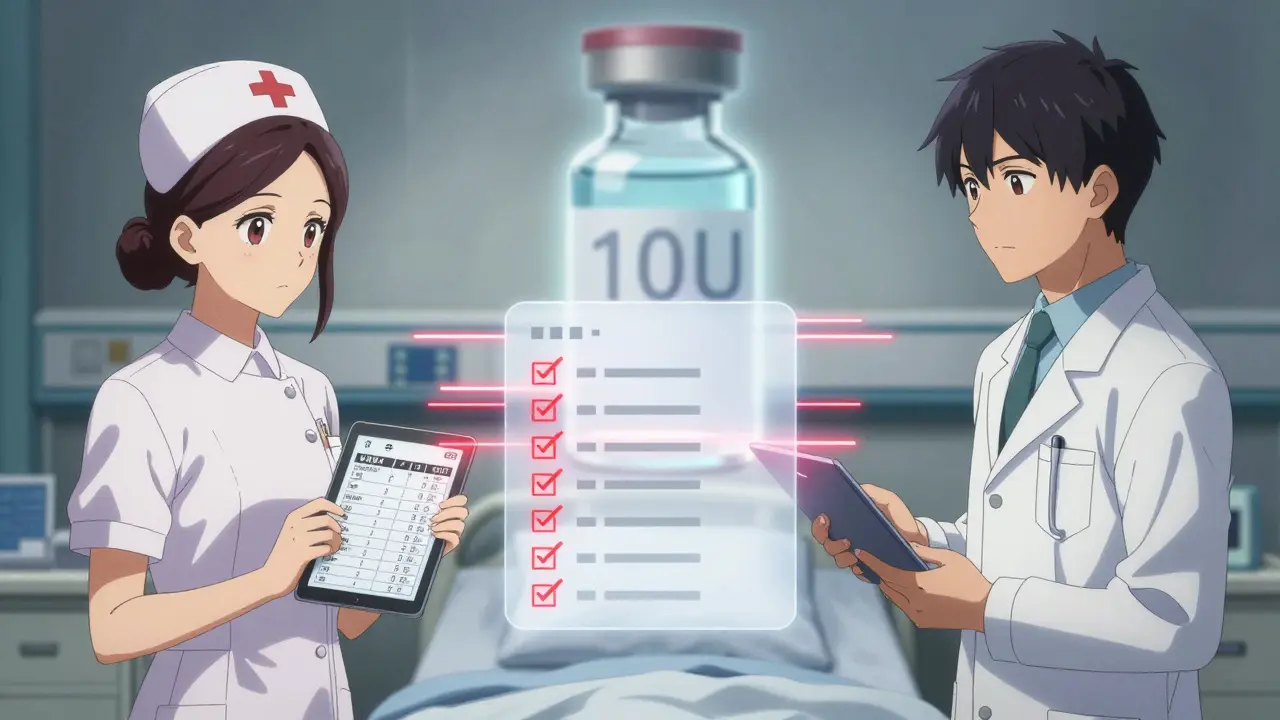
A patient’s dose doesn’t change in a vacuum. It’s often adjusted during a transition-discharge, ICU admission, shift change, or after a lab result. These are the exact moments when communication breaks down. A doctor writes “10U” for insulin, meaning ten units. The nurse reads it as one unit because the “.0” was missing. No one catches it. That’s not a typo-it’s a system failure. High-alert medications like insulin, heparin, opioids, and IV potassium are the biggest risks. One wrong dose can trigger cardiac arrest, severe hypoglycemia, or fatal bleeding. The Institute for Safe Medication Practices (ISMP) lists 19 of these drugs that demand extra safeguards. But here’s the catch: you don’t need to double-check every single dose. You need to double-check the right ones.The Two-Step Verification That Actually Works
For years, hospitals pushed universal double checks. Two nurses independently verify every medication. Sounds safe, right? But studies show that when double checks become routine, people start talking to each other, looking at the same screen, or just signing off because they’re tired. In one emergency department, compliance dropped to 45% during peak hours. The smarter approach? Targeted verification. Only use independent double checks where the risk is highest:- Insulin doses over 5 units or any change in basal rate
- Heparin infusions, especially when titrating by weight
- Opioid boluses for patients with renal impairment
- Any pediatric dose calculated by weight (must be precise to 0.1 mg/kg)
- Warfarin changes-always confirm INR within 24 hours
Barcode Scanning Isn’t Enough-But It’s Still Vital
Barcode medication administration (BCMA) systems scan the patient’s wristband and the drug’s barcode before giving it. They’re great for catching the wrong drug or wrong patient. In fact, they prevent 86% of those types of errors. But here’s the blind spot: they can’t catch the wrong dose. A nurse scans a vial of insulin labeled “100 units/mL” and enters “10 units.” The system says “match.” It doesn’t know if 10 units is too much for a 60-pound child or too little for someone in DKA. That’s where human judgment has to step in. The best practice? Combine both. Use BCMA for patient and drug verification, then do an independent double check for dose accuracy-especially for high-alert meds. The American Society of Health-System Pharmacists (ASHP) recommends this exact combo. Hospitals that do this see 40% fewer dose-related errors than those using either method alone.
How Communication Breaks Down-And How to Fix It
Miscommunication is the hidden cause behind 65% of serious medication errors, according to The Joint Commission. It’s not just about bad handwriting anymore. It’s about rushed phone calls, unclear handoffs, and vague documentation. Take this real example from a nurse on AllNurses.com: “I almost gave 10 units of insulin instead of 1 unit because the order said ‘10U’-no decimal. The double check caught it.” That’s a communication failure. The prescriber didn’t write “1.0U.” The pharmacist didn’t clarify. The nurse didn’t question it. The fix? Use structured communication tools like SBAR:- Situation: “Patient Smith, room 304, just had a fasting glucose of 280.”
- Background: “He’s on sliding scale insulin. Last dose was 8 units at 8 AM.”
- Assessment: “His insulin sensitivity dropped after antibiotics. He needs a higher dose.”
- Recommendation: “I recommend 12 units of lispro now. Can you confirm?”
The Hidden Cost: Alert Fatigue and Workload
Technology helps-but too much of it hurts. Nurses report getting 100+ alerts during a 12-hour shift. Most are false alarms: “This dose is outside normal range.” But the normal range was set for a 200-pound man, not a frail 70-year-old. So nurses learn to ignore them. A 2022 study found nurses only paid attention to 15% of BCMA alerts. That’s alert fatigue. And it’s deadly. The solution? Tune your systems. Set smart thresholds based on patient history. Don’t alarm for every small change. Only trigger alerts for high-risk deviations-like a 50% increase in heparin without an INR check. Also, protect time. Johns Hopkins Hospital added 15-20 minutes of “safety time” per nurse shift. No charting. No calls. Just time to verify doses, talk to patients, and pause before giving meds. Within a year, dose verification errors dropped 37%.
What Documentation Must Include
If you didn’t write it down, it didn’t happen. That’s the rule in healthcare. Every dose change verification needs three things in the record:- Time: When the verification occurred
- Verifiers: Names and credentials of both people who checked
- Context: Why the change was made-renal function, weight, lab results, patient symptoms
What’s Changing in 2026
New tools are coming. AI systems like Epic’s DoseRange Advisor now predict risky dose changes before they’re ordered-cutting inappropriate changes by 52% in a 12-hospital trial. Voice recognition tools let nurses say, “Verify insulin dose: 5 units subcutaneous for patient Smith,” and the system logs it automatically, saving 65% of documentation time. But the biggest shift? From universal checks to risk-based checks. Johns Hopkins’ Targeted Medication Verification protocol reduced nurse workload by 18% while cutting errors by 22%. That’s the future: fewer checks, smarter checks. The Joint Commission now requires reliable dose verification processes under NPSG.01.01.01-effective January 1, 2024. CMS will penalize hospitals with more than 0.5% dose verification error rates. This isn’t optional anymore.What You Can Do Today
You don’t need a $2 million system to make a difference. Start here:- Identify your top 5 high-alert medications. Make a list. Post it.
- Require independent double checks for those-no exceptions.
- Use SBAR for all dose change communications, especially during shift changes.
- Block 15 minutes per shift for verification. Protect it like a code blue.
- Review your BCMA alerts. Turn off the noise. Keep only the critical ones.
- Document every verification. Time, name, reason. No shortcuts.
What’s the difference between a single check and a double check for medication doses?
A single check means one person verifies the medication-patient, drug, dose, route, and time. A double check means two qualified staff members verify the same details independently, without talking to each other. Double checks are not meant for every dose. They’re used only for high-risk medications like insulin or heparin, where the consequences of error are severe. Studies show double checks catch 33% more dosing errors than single checks, especially for wrong-vial or wrong-dose mistakes.
Why do barcode systems sometimes miss dose errors?
Barcode systems scan the drug label and patient wristband to confirm identity. But they can’t verify if the dose amount is correct. For example, if a vial says 100 units/mL and the nurse enters 10 units, the system sees a match. It doesn’t know if 10 units is safe for a child or too low for someone in diabetic ketoacidosis. That’s why human verification is still essential-even with barcode tech.
Is it okay to skip verification during busy shifts?
No. Skipping verification, even during busy times, is one of the leading causes of preventable harm. A 2022 American Nurses Association survey found that 73% of nurses admitted skipping steps under pressure-and medication errors rose 22% during 12-hour shifts when verification was bypassed. Instead of skipping, advocate for safety time. Even 5 extra minutes per dose can save a life. Systems should be designed to support safety, not punish it.
How do I know if a dose change is high-risk?
A dose change is high-risk if it involves a high-alert medication (like insulin, heparin, or opioids), affects a vulnerable patient (elderly, pediatric, renal failure), or changes the route or concentration. Also, any change based on a lab result (like INR for warfarin) or weight-based calculation (pediatric doses) requires extra scrutiny. If you’re unsure, treat it as high-risk. Better safe than sorry.
What’s SBAR and why does it matter for dose changes?
SBAR stands for Situation, Background, Assessment, Recommendation. It’s a structured way to communicate during handoffs or when requesting a dose change. Instead of saying, “Give him more insulin,” you say: “Patient is 78, fasting glucose 310, on sliding scale, last dose was 8 units-glucose hasn’t dropped. Recommend 12 units now.” This reduces ambiguity. Studies show SBAR cuts miscommunication errors by 41% during transitions of care.
Can AI replace human verification for dose changes?
AI can flag risky changes before they happen-like Epic’s DoseRange Advisor, which reduced inappropriate doses by 52% in a trial. But AI can’t replace human judgment. It doesn’t know if a patient is dehydrated, has a new infection, or is confused. It can’t ask, “Are you sure?” Human verification is still needed to interpret context, spot anomalies, and speak up when something feels wrong. AI supports. Humans decide.

Patrick Merrell
January 26, 2026 AT 23:22This is exactly why I refuse to trust automated systems alone. I've seen too many nurses scan a vial and just assume it's right. One time, a kid got 10x the insulin dose because the barcode matched but the decimal was missing. No one caught it until the seizure started. Double checks aren't bureaucracy-they're the last line of defense.
Aurelie L.
January 28, 2026 AT 04:17They don't need more rules. They need fewer alerts and more time.