Imagine you’re taking five different pills every day. One for your blood pressure, one for your thyroid, another for your bones, plus an antibiotic and a pain reliever. You don’t feel worse - but you also don’t feel better. Your doctor says everything looks fine on paper. But something’s off. You’re tired all the time. Your bones still ache. Your blood pressure won’t budge. What’s missing? Timing.
Most people think drug interactions mean one pill cancels out another. That’s true sometimes. But the real hidden danger? When two drugs are taken too close together - not because they’re incompatible, but because of when you take them. This isn’t guesswork. It’s science. And it’s preventable.
Why Timing Matters More Than You Think
Not all drug interactions are created equal. Some happen because drugs compete for the same enzyme in your liver. Those? Timing won’t help. But a huge chunk - up to 30% - are time-dependent. That means if you take them at the right distance apart, they work fine. Take them together? You’re wasting half your treatment.
Take iron supplements and levothyroxine, for example. Levothyroxine is the medicine that keeps your thyroid running. Iron? It’s essential for energy. But if you take them together, your body absorbs less than 5% of the thyroid hormone. That’s not a minor drop. That’s enough to leave you exhausted, cold, and depressed - even if your dose is perfect. Separate them by just four hours, and absorption jumps back to 95%. That’s not magic. That’s pharmacokinetics.
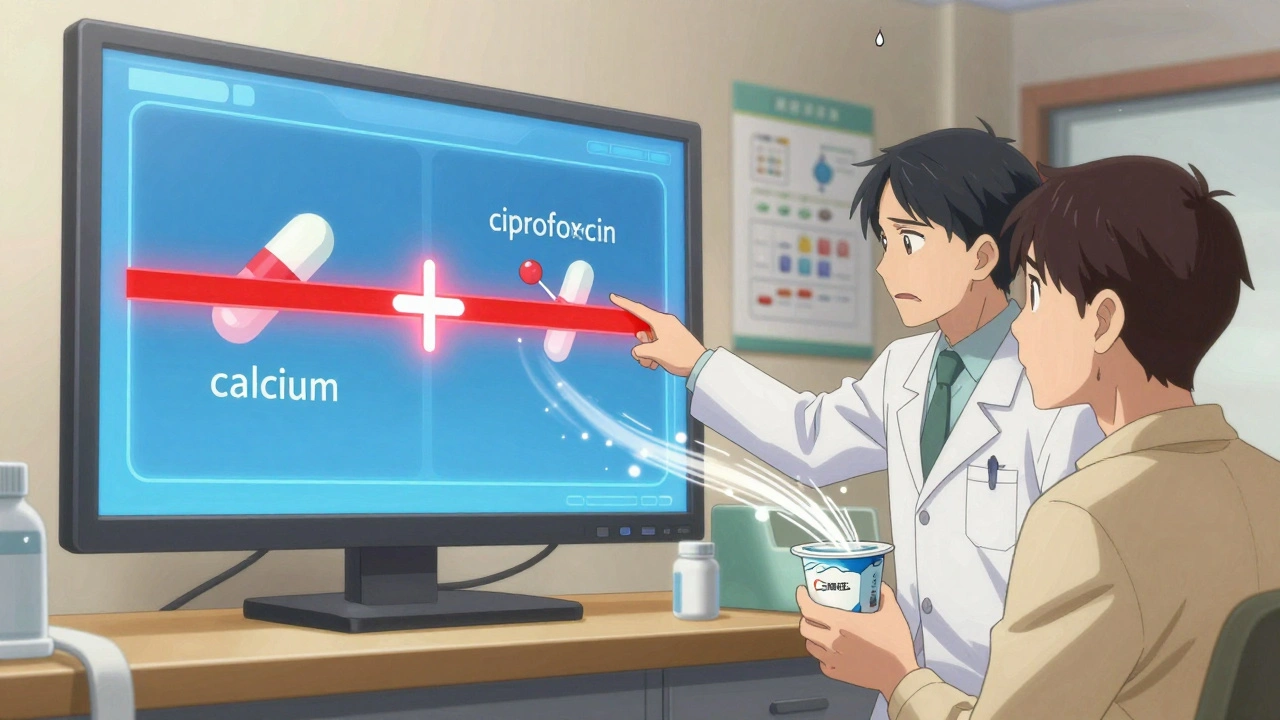
Same with antibiotics like ciprofloxacin. Take them with milk, calcium pills, or antacids? The calcium binds to the antibiotic in your gut. Up to 90% of the drug gets blocked. You think you’re fighting the infection. You’re not. You’re just swallowing expensive chalk. Two hours apart? The antibiotic works as intended.
This isn’t theoretical. In 2021, a study at UCSF Medical Center showed that when pharmacists started timing iron and proton pump inhibitors correctly in elderly patients, cases of iron-deficiency anemia dropped by 32% in just 18 months. That’s real people getting better - not because they got a new drug, but because they took them at the right time.
The Top 5 Time-Dependent Interactions You Need to Know
Some interactions are so common, they’re practically routine. Here are the big five you’re likely to encounter - and exactly how to fix them:
- Levothyroxine + Iron/Calcium/Magnesium: Take thyroid medicine on an empty stomach, first thing in the morning. Wait at least 4 hours before taking any supplement with iron, calcium, or magnesium (including antacids or multivitamins).
- Fluoroquinolone antibiotics (ciprofloxacin, levofloxacin) + Antacids, Dairy, or Calcium: Separate by 2 hours. No exceptions. Don’t take your antibiotic with yogurt or a Tums.
- Bisphosphonates (alendronate, risedronate) + Food or Other Medications: Take on an empty stomach with a full glass of water. Wait 30 minutes before eating, drinking, or taking anything else. Even coffee can block absorption.
- Tetracycline antibiotics + Calcium, Magnesium, Aluminum, or Zinc: These include doxycycline and minocycline. Avoid dairy, antacids, and iron pills for at least 2-3 hours before and after.
- Proton pump inhibitors (omeprazole, esomeprazole) + Atazanavir (HIV drug): PPIs reduce stomach acid, which atazanavir needs to absorb. If you’re on both, your doctor may need to adjust the dose - timing alone won’t fix this one.
These aren’t rare. They’re daily occurrences in hospitals, clinics, and homes. And they’re avoidable.
What Timing Won’t Fix - And What to Do Instead
Timing only works for absorption-based interactions. It doesn’t help with metabolic ones. That’s when one drug changes how your liver breaks down another.
Example: Warfarin (a blood thinner) and metronidazole (an antibiotic). Metronidazole shuts down the liver enzyme that clears warfarin. The result? Too much warfarin in your blood. That’s not about when you take them - it’s about how your body processes them. Take them 12 hours apart? Still dangerous. The fix? Either stop the antibiotic, switch to another one, or reduce the warfarin dose under close monitoring.
Same goes for grapefruit juice and statins. Grapefruit blocks an enzyme that breaks down atorvastatin and simvastatin. No matter when you drink it - morning, noon, night - it still builds up in your system. The only safe move? Avoid grapefruit entirely.
Bottom line: Timing is powerful - but only for certain interactions. If you’re unsure, ask your pharmacist. They have access to databases like Lexicomp that tell you exactly which interactions are timing-sensitive and which require a different approach.
How to Make Timing Work in Real Life
You know what to do. But life isn’t a textbook. You’re busy. You forget. You travel. You sleep in. So how do you actually make this stick?
Start with a full medication review. Write down every pill, supplement, and over-the-counter drug you take - including vitamins, herbal teas, and pain relievers. Don’t skip anything. Even the ‘harmless’ ones.
Next, use a pill organizer with separate compartments for morning, afternoon, evening, and night. Not the cheap kind with four slots. Get one with 7 compartments per day - or better yet, one with time-labeled slots (7 AM, 12 PM, 7 PM, 11 PM).
Then, use an app. Medisafe, MyTherapy, or even Google Keep with custom alarms can remind you not just to take your pills, but when to wait. Set an alarm: ‘Take thyroid - wait 4 hours before iron.’ It sounds silly. But 57% of patients in a 2021 trial improved adherence using apps like these.
For older adults or those on 10+ medications, ask your pharmacist for a printed schedule. Color-code it. Red for ‘must wait 4 hours,’ blue for ‘take with food,’ green for ‘anytime.’ Tape it to your bathroom mirror. Keep a copy in your wallet.
And here’s the hard truth: If your doctor doesn’t mention timing, ask. Most don’t. A 2023 Medscape survey found that 78% of primary care doctors find managing multiple timing requirements ‘moderately to severely difficult.’ That doesn’t mean it’s impossible. It means you need to be your own advocate.

The Bigger Picture: Why This Is a System Problem
This isn’t just about you forgetting to wait two hours. It’s about how medicine is designed.
Most drug labels don’t mention timing. Only 27% of prescriptions now include separation instructions - and even those are often buried in fine print. Hospitals use electronic systems that flag potential interactions - but 45% of their alerts are false positives. That means doctors start ignoring them. Patients get confused.
Meanwhile, the FDA now recommends timing for 17 high-risk combinations - including clarithromycin and colchicine, where separating them by 2 hours cuts toxicity risk by 60%. But if your pharmacist doesn’t know, or your doctor didn’t write it down, you’re left guessing.
The solution? Better labeling. Better training. Better tech. But until then, you’re the most important link in the chain.
Every year, 115,000 to 178,000 preventable drug reactions happen in the U.S. alone. A huge chunk of those are from timing errors. That’s not just statistics. That’s people in hospitals because they took their calcium pill with their thyroid medicine. That’s someone with a broken hip because their bone drug didn’t work. That’s avoidable.
You don’t need to be a doctor. You just need to be informed. And you need to ask.
What to Do Next
Here’s your simple action plan:
- Write down every medication and supplement you take - including doses and times.
- Check the top 5 interactions above. Do any match yours?
- Call your pharmacist. Ask: ‘Are any of my medications time-sensitive?’ They’ll check it for free.
- Set phone alarms for separation windows. Even if you think you’ll remember - set them anyway.
- Ask your doctor at your next visit: ‘Have you checked if any of my meds need spacing?’
Timing isn’t about being perfect. It’s about being smarter. You’re not just taking pills. You’re managing a system. And systems work best when every piece is in the right place - at the right time.


kevin moranga
December 13, 2025 AT 14:02Man, I wish I’d known this five years ago. I was taking my levothyroxine with my calcium gummies like it was breakfast cereal. No wonder I felt like a zombie. Once I started waiting 4 hours? I swear I got my energy back. Like, I started walking the dog again. My wife thought I was cheating on her with a new hobby. It’s not magic-it’s just not being dumb with your meds.
Also, stop taking your probiotics with your antibiotics. That’s another one people forget. Space ‘em out. Your gut will thank you.
Alvin Montanez
December 13, 2025 AT 20:02People think they’re ‘doing their part’ by taking pills, but half of them are just poisoning themselves with poor timing. This isn’t rocket science-it’s basic biology. If you can’t follow a 2-hour window, maybe you shouldn’t be on five meds. You’re not special. Your body doesn’t care about your schedule. It cares about absorption. Stop making it harder.
And no, ‘I forgot’ is not an excuse. Set alarms. Use a pillbox. Or stop complaining about being tired all the time.
Keasha Trawick
December 15, 2025 AT 16:32Okay, let’s talk about the pharmacokinetic ballet happening in your GI tract. Levothyroxine is a diva-it needs an empty stage, no calcium divas, no iron understudies, no magnesium stagehands. You dump them all together? Chaos. Absorption plummets. Thyroid hormone becomes a ghost in your bloodstream.
And cipro? It’s like a VIP guest at a club-calcium is the bouncer. If they show up together? You’re denied entry. Two hours apart? The bouncer steps aside. The drug gets in. The infection gets wrecked.
This isn’t just advice-it’s molecular choreography. And if you’re not rehearsing it? You’re just dancing with ghosts.
Webster Bull
December 17, 2025 AT 08:24Timing > dosage sometimes. Seriously. I used to take my omeprazole with my iron. Felt like crap. Then I spaced ‘em. Magic. Don’t overthink it. Just set a damn alarm. Your body’s not dumb. You are if you don’t listen.
ps. yes i spelled ‘em wrong. sue me.
Emma Sbarge
December 18, 2025 AT 00:32Why are we letting drug companies get away with this? Labels should scream ‘WAIT 4 HOURS’ in red, blinking letters. Not buried in 8-point font next to ‘may cause drowsiness.’ This is negligence. We’re paying for these drugs, not begging for them. If they don’t want us dying from timing errors, they should make it impossible to mess up.
And no, ‘ask your pharmacist’ isn’t a solution. Most pharmacists are overworked. This is a systemic failure. Fix the system.
Tommy Watson
December 19, 2025 AT 04:59Wait, so I gotta wait 4 hours after my thyroid med to take my multivitamin? That’s ridiculous. I take it at night. Why can’t I just take it with the thyroid in the morning? It’s all the same stuff. Why make it harder? I’m not a robot.
Also, who even has time for this? I’m a single dad. I barely remember to brush my teeth.
Donna Hammond
December 20, 2025 AT 22:10Tommy, I get it. Life’s messy. But you don’t have to be perfect-you just have to be consistent. Start with one change. Maybe move your multivitamin to bedtime. That’s 8 hours from your thyroid med. Perfect. No need to rearrange your whole day.
And if you’re a single dad, you’re already a superhero. Use your phone. Set one alarm: ‘Thyroid-wait till after breakfast.’ That’s it. One tiny win. Then build from there. You’ve got this.
Richard Ayres
December 21, 2025 AT 20:16This is a profoundly important topic that deserves far more public attention. The disconnect between clinical knowledge and patient practice is alarming. Pharmacokinetic principles are not obscure-they’re foundational. Yet they are routinely omitted from patient education.
I commend the author for highlighting the distinction between absorption-based and metabolic interactions. Too many patients conflate the two, leading to inappropriate self-adjustments. The call for pharmacist involvement is not just reasonable-it’s essential.
Karen Mccullouch
December 23, 2025 AT 08:40Ugh. I’ve been taking my iron and thyroid together for YEARS. And I’m still alive. So what’s the big deal? Maybe this is just fear-mongering by Big Pharma to sell more apps and pill organizers. I don’t need an alarm to take my pills. I have a brain.
Also, why do we trust pharmacists more than doctors? They’re just the ones who hand out the pills. Not the ones who actually know what’s wrong with me.
Michael Gardner
December 23, 2025 AT 17:01Actually, the 30% statistic is misleading. That study was observational. No control group. Also, UCSF is a rich hospital with dedicated pharmacists. Most clinics don’t have that luxury. And what about patients on 12 meds? You can’t space everything 4 hours apart. It’s not practical. This advice sounds great on paper. In real life? It’s a nightmare.
Tom Zerkoff
December 25, 2025 AT 01:51While the practical guidance is commendable, I would urge readers to consider the broader implications of polypharmacy in aging populations. The cognitive load imposed by multiple timing requirements is not trivial. The burden often falls disproportionately on vulnerable individuals who lack social or technological support.
It is imperative that healthcare systems move beyond individual responsibility and implement structural solutions-automated dispensers, integrated EHR alerts, and pharmacist-led medication reconciliation programs. The onus should not rest solely on the patient.
Yatendra S
December 26, 2025 AT 15:34life is like a river… meds are stones in it… timing is the current… if you put the stones too close, the water can’t flow… 🌊💊
so… breathe… set alarm… and let your body be the temple… 🙏