Steroid-Induced Osteoporosis Prevention Calculator
Your Treatment Assessment
Recommended Treatment
Enter your information above to see your recommended treatment plan.
Important: This tool provides general guidance only. Always consult with your doctor for personalized medical advice and treatment.
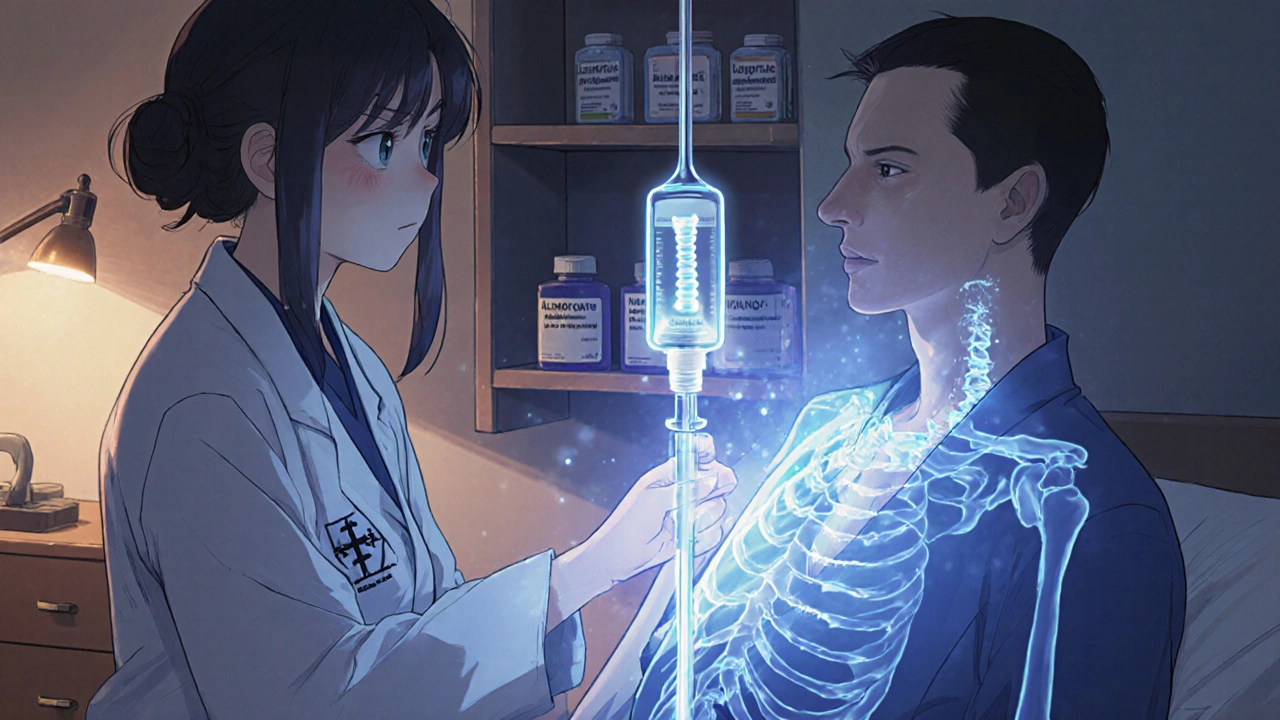
Why Steroids Don’t Just Affect Inflammation-They Also Break Down Your Bones
If you’re taking steroids like prednisone for asthma, rheumatoid arthritis, or lupus, you’re probably aware of the side effects: weight gain, mood swings, trouble sleeping. But there’s another silent risk that doesn’t get talked about enough-your bones are thinning, and fast.
Glucocorticoid-induced osteoporosis (GIOP) is the most common form of secondary osteoporosis. Studies show that 30% to 50% of people on long-term steroid therapy lose enough bone density to put them at high risk for fractures. And it doesn’t take years. Bone loss can start within 3 to 6 months of starting treatment. By the end of the first year, 12% of patients on doses of 7.5 mg or more of prednisone daily will already have suffered a vertebral fracture.
Unlike regular osteoporosis, which happens slowly as we age, GIOP hits hard and fast. Steroids don’t just reduce calcium absorption-they shut down bone-building cells (osteoblasts) and wake up bone-eating cells (osteoclasts). This dual attack means your skeleton loses strength from both sides.
Step One: Calcium and Vitamin D Are Non-Negotiable
Before you even think about pills that stop bone loss, you need to lay the foundation. That’s calcium and vitamin D.
The American College of Rheumatology (ACR) recommends 1,000 to 1,200 mg of calcium daily and 600 to 800 IU of vitamin D for anyone starting long-term steroid therapy (3 months or more at 2.5 mg prednisone or higher). If your vitamin D level is below 30 ng/mL-which is common-you should bump it up to 800-1,000 IU daily.
Where do you get this? Food helps, but not enough. One cup of milk has about 300 mg calcium. A serving of yogurt, 250 mg. A cup of cooked spinach? 240 mg-but your body can’t absorb half of it because of oxalates. That’s why supplements are often necessary.
Vitamin D is trickier. Even in sunny places like Auckland, many people are deficient, especially if they’re indoors a lot or cover up for medical reasons. Your body makes vitamin D from sunlight, but steroids interfere with how your skin uses it. A blood test is the only way to know if you’re getting enough.
Don’t just take them randomly. Take calcium in divided doses-no more than 500 mg at a time-because your body can’t absorb more than that efficiently. And always take vitamin D with a meal that has fat. It’s a fat-soluble vitamin. No fat? It passes right through you.
Step Two: Bisphosphonates-The First-Line Defense
If you’re on steroids long-term and you’re over 40, or you’ve had a fracture before, you need more than supplements. You need a drug that actually stops bone loss.
Bisphosphonates are the most studied, most trusted, and most affordable option. They work by slowing down the osteoclasts-the cells that chew up bone. The two most common oral bisphosphonates are alendronate (Fosamax) and risedronate (Actonel).
Here’s what the data shows:
- Alendronate increases spine bone density by 3.7% in one year-while placebo groups lose bone.
- Risedronate cuts vertebral fracture risk by 70% in the first year.
- Both reduce fracture risk by 41% to 56% overall.
They’re not perfect. About 15% to 30% of people get stomach upset, heartburn, or esophageal irritation. That’s why dosing matters. Take them first thing in the morning, on an empty stomach, with a full glass of water. Stay upright for at least 30 to 60 minutes. No lying down. No eating. No other meds.
If you can’t stick to that routine, you’re not alone. Half of people stop taking oral bisphosphonates within a year. That’s why zoledronic acid (Reclast) is a game-changer. It’s an IV infusion given once a year. No daily pills. No waiting around after swallowing. Studies show it improves spine bone density even more than oral versions-and improves adherence by 38%.
When Bisphosphonates Aren’t Enough: Teriparatide
Not everyone responds the same. If you’re already at high risk-say, you’ve had a previous fracture, your bone density is below -2.5 on the T-score, or you’re under 40 with multiple risk factors-bisphosphonates might not be strong enough.
That’s where teriparatide (Forteo) comes in. Unlike bisphosphonates, which slow bone loss, teriparatide actually builds new bone. It’s a synthetic version of parathyroid hormone. You inject it daily under your skin.
The numbers speak for themselves:
- In the ACTIVE trial, only 0.6% of patients on teriparatide had new vertebral fractures vs. 6.1% on alendronate.
- Lumbar spine bone density increased by 16.2% with teriparatide over 18 months-compared to just 4.3% with alendronate.
But there’s a catch. It costs about 10 times more than generic bisphosphonates-around $2,500 a month in the U.S. And you can only use it for 2 years total in your lifetime because of a small risk of bone cancer in rats (no proven risk in humans after 15+ years of use).
It’s not for everyone. Avoid teriparatide if you’ve had radiation to your bones, Paget’s disease, or bone cancer. But if you’re young, severely osteoporotic, and haven’t responded to bisphosphonates? It’s often the best shot you’ve got.
Other Options: Denosumab and Newer Drugs
Denosumab (Prolia) is another option. It’s a monthly or twice-yearly injection that blocks a protein called RANKL, which tells bone cells to break down bone. It reduces vertebral fracture risk by 79%-better than bisphosphonates.
It’s great for people who can’t take bisphosphonates because of kidney problems or stomach issues. But if you stop denosumab suddenly, you can lose bone faster than before. That means you need a transition plan-usually switching to a bisphosphonate or teriparatide.
Then there’s abaloparatide, a newer drug approved in 2022. It’s similar to teriparatide but appears to build bone even faster. In trials, it increased spine density by 8.6% more than teriparatide at 18 months. But it’s even more expensive and not yet widely used.
Right now, bisphosphonates still make up 65% of the GIOP treatment market-not because they’re the best, but because they’re affordable, proven, and widely available.
Who Needs What? A Simple Guide
Not everyone needs the same treatment. Here’s how to think about it:
- All patients on steroids for 3+ months at ≥2.5 mg prednisone/day → start calcium + vitamin D immediately.
- Patients over 40 → add oral bisphosphonate (alendronate or risedronate) unless contraindicated.
- Patients under 40 with prior fracture or T-score ≤-2.5 → consider teriparatide or denosumab.
- Patients with kidney problems (eGFR < 30) → avoid oral bisphosphonates. Use denosumab or teriparatide.
- Patients who can’t tolerate pills → switch to annual zoledronic acid infusion.
Don’t wait for a fracture to happen. By then, it’s too late. Prevention starts on day one of steroid treatment.

Monitoring and Long-Term Risks
Once you start treatment, you need to track your progress. Get a DXA scan (bone density test) at the start, then again at 12 months. If your bone density drops more than 5% in a year, your treatment plan needs adjusting.
Long-term bisphosphonate use (over 3-5 years) can lead to rare but serious problems: atypical femur fractures (a type of thigh bone break that happens with little or no trauma) and osteonecrosis of the jaw (bone death in the jaw, often after dental work). The risk is low-about 1 in 10,000 to 1 in 100,000 per year-but it’s real.
If you’ve been on bisphosphonates for 5 years or more, talk to your doctor about a “drug holiday.” Pause the medication for a year or two while you monitor bone density. Sometimes, your bones can recover enough to stay protected without constant drugs.
Why So Many People Still Don’t Get Treated
Here’s the uncomfortable truth: despite clear guidelines, only 19.3% of patients on long-term steroids actually get bone protection within three months of starting treatment. That’s not just a gap in care-it’s a failure of the system.
Doctors are busy. Patients don’t know the risk. Pharmacies don’t flag it. Insurance doesn’t push it. And many people think, “I feel fine, so why bother?”
But osteoporosis doesn’t hurt until you break a bone. And once you fracture a vertebra, your life changes. You lose height. You get chronic pain. You can’t walk without fear. Your risk of another fracture skyrockets.
Prevention isn’t optional. It’s the difference between living with steroids-and living well despite them.
What’s Next? The Future of Bone Protection
Research is moving fast. One big question: Should we use teriparatide first, then switch to a bisphosphonate? The SWAN trial (NCT04123456) is testing this exact idea. Early results suggest this “sequential therapy” might give you more bone gain than either drug alone.
Cost is also changing. Generic bisphosphonates are dirt cheap. But as newer drugs like abaloparatide become available and patents expire, prices may drop. By 2030, osteoanabolic drugs could make up 30% of the GIOP market.
But for now, the best advice remains simple: start calcium and vitamin D. Get your bone density checked. If you’re at risk, start a bisphosphonate. Don’t wait. Don’t assume you’re fine. Your bones are counting on you.


Matthew Peters
November 19, 2025 AT 22:29Liam Strachan
November 21, 2025 AT 06:39Gerald Cheruiyot
November 21, 2025 AT 20:27Michael Fessler
November 22, 2025 AT 22:45daniel lopez
November 24, 2025 AT 04:00Nosipho Mbambo
November 25, 2025 AT 08:33Katie Magnus
November 27, 2025 AT 04:21King Over
November 27, 2025 AT 16:26Johannah Lavin
November 28, 2025 AT 13:04Ravinder Singh
November 30, 2025 AT 09:24Russ Bergeman
December 1, 2025 AT 23:58Ravi boy
December 2, 2025 AT 16:57Matthew Karrs
December 3, 2025 AT 01:22