When you start a new medication, it’s normal to wonder: is this feeling something the drug is causing, or is it just my body adjusting? Maybe you’ve got a headache after taking your blood pressure pill, or your skin broke out after starting a new antibiotic. You don’t want to ignore it - but you also don’t want to panic over something harmless. That’s where a symptom diary comes in. It’s not just a notebook. It’s your best tool to figure out if a drug is truly causing problems - and to help your doctor make faster, smarter decisions.
Why a Symptom Diary Matters
Most people remember the big stuff - like a rash or vomiting. But what about the small, weird things? A sudden dizziness at 3 p.m. that fades by dinner. A feeling of tightness in your chest after taking your pill with lunch. A strange taste in your mouth that lasts five minutes. These are the clues doctors need to spot a real drug reaction. Without them, you’re guessing. And guesswork leads to misdiagnosis. A 2023 study from Enjuris showed a patient involved in a car accident was wrongly blamed for poor judgment - when the real cause was dizziness from a newly prescribed painkiller. The patient hadn’t recorded the timing. No one knew the dizziness started exactly 40 minutes after taking the pill. That’s the power of a diary. It turns vague feelings into hard evidence. The FDA and NIH agree: if you’re tracking suspected drug reactions, writing things down as they happen cuts down on false alarms by 62%. That means fewer unnecessary tests, fewer medication changes based on guesswork, and more accurate diagnoses.What to Write Down - The 9 Must-Have Details
A good symptom diary isn’t just a list of “I felt bad.” It’s a timeline. Here’s exactly what you need to record for every reaction:- Date and time - Write the exact minute you took the medication. Don’t say “this morning.” Say “9:15 a.m.”
- Medication name and dose - Include the brand and generic name. If you took 25 mg of lisinopril, write that. If you took two 500 mg ibuprofen tablets, write that too.
- How you took it - Swallowed with water? Chewed? Applied to skin? Taken with food? All of this matters.
- Other meds or supplements - Even if they’re “just” vitamins, fish oil, or herbal tea. Drug interactions are common and often missed.
- Symptom description - Be specific. Don’t say “felt weird.” Say “sharp pain in left chest, radiating to left arm, started 25 minutes after pill.”
- Where the symptom happened - Head? Stomach? Hands? Skin? Be anatomical.
- When it started - How long after taking the drug? 10 minutes? 2 hours? 12 hours?
- How long it lasted - Did it fade in 15 minutes? Last all day? Come and go?
- What you did to fix it - Did you lie down? Take antihistamines? Drink water? Did it help?
- Environmental factors - Were you stressed? Hot? Exercising? Had you slept poorly? These can mix with drug effects.
For skin reactions, take a photo. The European Medicines Agency found that adding a picture of a rash or swelling increases diagnostic accuracy by 78%. A blurry phone snap is better than no photo at all.
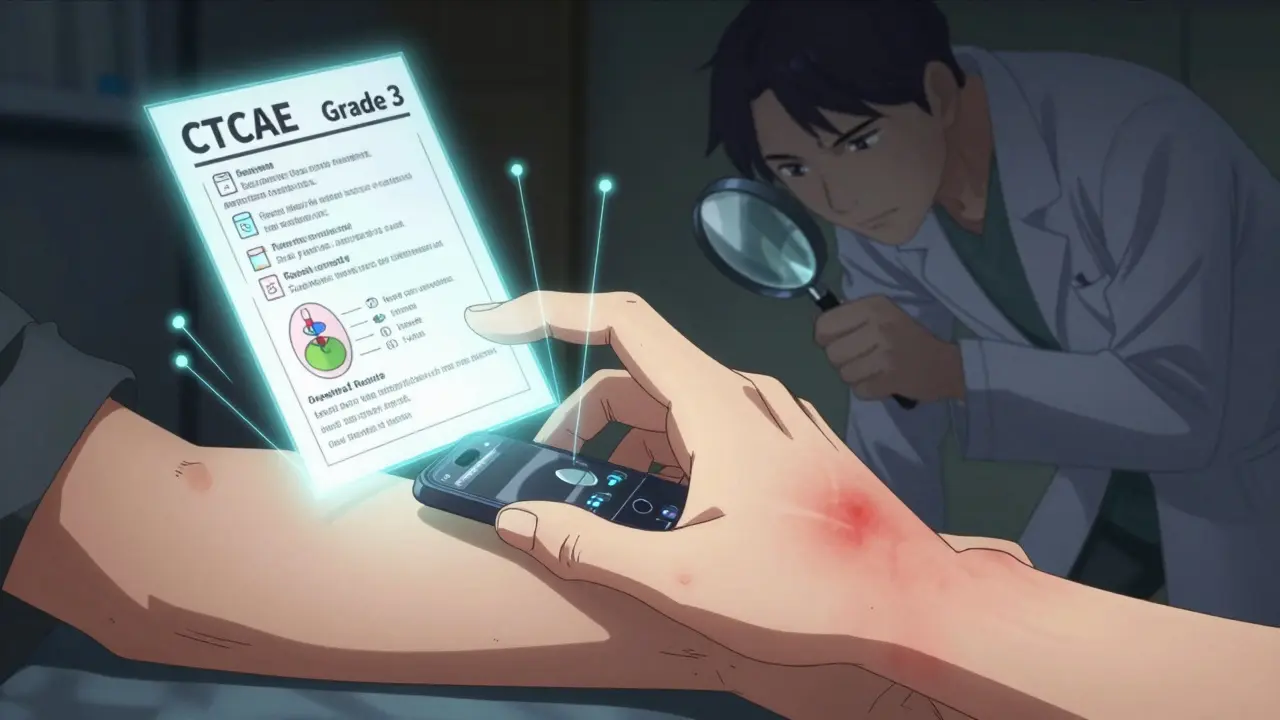
How to Rate Your Symptoms - The CTCAE Scale
Not all symptoms are equal. A mild headache is different from a dangerous drop in blood pressure. Use the Common Terminology Criteria for Adverse Events (CTCAE) version 5.0 to rate severity:- Grade 1 (Mild) - Asymptomatic or mild symptoms; no intervention needed. Example: slight nausea, no vomiting.
- Grade 2 (Moderate) - Minimal, local, or noninvasive intervention indicated. Example: vomiting once a day, dizziness that affects walking.
- Grade 3 (Severe) - Medically significant but not immediately life-threatening. Example: severe diarrhea, high fever, fainting.
- Grade 4 (Life-threatening) - Urgent intervention needed. Example: low blood pressure requiring IV fluids, trouble breathing.
- Grade 5 (Death) - Related to the drug.
Don’t overthink it. If you’re worried enough to write it down, it’s at least Grade 2. Write the grade next to each symptom. It helps your doctor see the pattern fast.
When to Write - Timing Is Everything
Your memory is unreliable. Studies show people forget key details after just 48 hours. That’s why the NIH says you must write things down within 72 hours - and ideally within 15 minutes for sudden reactions. Set a routine:- Record every time you take a medication - right after you swallow it.
- Check in every 30 minutes after taking a new drug, especially in the first 24 hours.
- If you feel something odd, write it down immediately. Don’t wait until bedtime.
- Review your diary every Sunday with your doctor or pharmacist.
Use your phone’s alarm. Set one for 10 minutes after each dose. It’s not nagging - it’s saving your health.
Paper vs. App - Which One Works Better?
You can use a notebook. But most people quit after three days. Why? It’s too much work. Apps like Medisafe, CareClinic, and MyTherapy make it easier:- They auto-log the time you take your meds.
- They let you tap a button to record symptoms - no typing needed.
- They show graphs of when symptoms happen relative to your doses.
- They send reminders to log your symptoms.
A 2023 Scripps Research study found that 57% of people gave up on paper diaries within 72 hours. Only 22% quit using apps with reminders. The difference? Convenience.
If you’re tech-savvy, go digital. If you hate screens, use a printed template with checkboxes for common symptoms (headache, nausea, rash, dizziness). Pre-made forms increase completion rates by 67%.
What Not to Do
Most people make the same mistakes:- Writing down every little thing - Not every burp or yawn is a reaction. Focus on new, unusual, or worsening symptoms. Overloading your diary with expected side effects (like mild drowsiness from a sedative) makes it harder to spot the real danger.
- Forgetting other meds - You might think your multivitamin doesn’t matter. It does. Some vitamins interact with blood thinners, antidepressants, or statins.
- Waiting until your appointment - If you wait a week to write it down, you’ll forget the timing. And timing is everything.
- Not showing it to your doctor - A diary only helps if someone sees it. Bring it to every visit. Print it out or show it on your phone.
Real Stories - What Works
On Reddit, a user named u/MedTracker89 wrote: “My neurologist kept saying my dizziness was from stress. I showed him my 14-day diary. Every time I took levodopa, the dizziness hit 45 minutes later. He changed my dose within two days.” Another patient, on Drugs.com, said: “I used to feel guilty for complaining. Now I have proof. My pharmacist told me my rash was likely from the new antibiotic - not my allergies. We switched drugs and it cleared up in 48 hours.” These aren’t rare. In a survey of 1,247 patients, 68% said their symptom diary improved their doctor visits. 42% had their medication changed because of what they recorded.
What Happens Next?
Your doctor might not say much when you hand them the diary. But they’ll be thinking: “This is the clearest data I’ve seen in months.” They might:- Adjust your dose
- Switch you to a different drug
- Order a blood test to check for organ stress
- Refer you to an allergist or dermatologist
- Report the reaction to the FDA’s adverse event database
That last one matters. Your diary isn’t just for you - it helps improve drug safety for everyone.
Final Tip: Keep It Simple, Keep It Going
You don’t need to be perfect. Miss a day? Just start again. Forgot to take a photo? Write “rash on forearm” as best you can. The goal isn’t perfection. It’s pattern recognition. The most successful diaries are the ones that are easy to maintain. Use an app. Use a printed form. Use a notebook with sticky notes. But don’t stop. Because the next time you feel something odd - you’ll know exactly what to do.What counts as a drug reaction worth writing down?
Any new, unusual, or worsening symptom that appears after starting a new medication. Don’t write down expected side effects like mild drowsiness from a sleep aid - unless they get worse. Focus on symptoms you didn’t have before, especially if they’re severe, sudden, or affect your daily life - like chest tightness, swelling, trouble breathing, rash, confusion, or fainting.
How long should I keep my symptom diary?
Keep it for at least two weeks after starting a new drug. For chronic medications, keep it ongoing. If you notice a pattern, keep the diary even after the reaction stops - it helps if the issue returns. Many doctors ask for 30 days of data before making changes.
Can I use my phone’s health app instead?
Apple Health and Google Fit can track medication times and some symptoms, but they’re not designed for drug reactions. Use a dedicated app like CareClinic or MyTherapy - they’re built for this. They let you link symptoms to specific drugs, add photos, and generate reports your doctor can read.
What if I don’t remember the exact time I took my pill?
Estimate as best you can. Write “around 8 a.m.” if you’re unsure. It’s better than nothing. But try to be consistent - always log right after you take the pill. Set a phone alarm to remind you. Timing errors are the #1 reason diaries get dismissed by doctors.
Should I show my diary to my pharmacist too?
Yes. Pharmacists are trained to spot drug interactions and side effects. They can tell you if your symptom matches known reactions for that drug. Many pharmacies now offer free medication review sessions - bring your diary. It can prevent dangerous mistakes before they happen.
Is it too late to start a diary if I’ve been on the drug for months?
No. Even if you’ve been on the medication for months, start now. Some reactions develop over time. If you’ve had a new symptom recently, document it from today. You might catch a delayed reaction or a drug interaction that just started because you added a new supplement.
What if my doctor ignores my diary?
If your doctor dismisses your diary, ask: “Can you explain why this pattern doesn’t look like a reaction?” If they still won’t act, get a second opinion. Your symptoms matter. A symptom diary is a recognized tool by the FDA and NIH - you have the right to be heard.


Randolph Rickman
December 16, 2025 AT 21:21Josias Ariel Mahlangu
December 17, 2025 AT 17:22Arun ana
December 19, 2025 AT 13:33Kayleigh Campbell
December 20, 2025 AT 03:17Kim Hines
December 20, 2025 AT 21:33SHAMSHEER SHAIKH
December 22, 2025 AT 18:35James Rayner
December 23, 2025 AT 10:10anthony epps
December 25, 2025 AT 08:32Andrew Sychev
December 26, 2025 AT 08:34Dan Padgett
December 26, 2025 AT 13:08Hadi Santoso
December 27, 2025 AT 04:32Joanna Ebizie
December 28, 2025 AT 11:02sue spark
December 29, 2025 AT 00:18Tiffany Machelski
December 29, 2025 AT 02:40