Gut-Skin Connection: Nodular Acne Risk Calculator
Your Gut-Skin Risk Assessment
Probiotic Recommendations
| Strain | Dose | Benefit |
|---|---|---|
| Lactobacillus rhamnosus | 1 × 10⁹ CFU/day | Reduces nodule count |
| Bifidobacterium breve | 5 × 10⁸ CFU/day | Improves redness |
| Streptococcus thermophilus | 2 × 10⁹ CFU/day | Reduces IL-6 levels |
Key Takeaways
- Imbalanced gut bacteria can worsen nodular acne by triggering systemic inflammation.
- Dietary choices that support a diverse gut microbiome often lead to clearer skin.
- Targeted probiotic strains such as Lactobacillus rhamnosus have shown measurable reductions in lesion count.
- Addressing leaky gut, stress, and hormonal spikes helps break the acne‑gut feedback loop.
- Combining gut‑friendly foods with dermatological care yields the most sustainable results.
What Is Nodular Acne?
Nodular acne is a severe form of acne characterized by large, painful lumps that sit deep within the skin. Unlike surface pimples, these nodules form when the hair follicle becomes clogged with excess oil, dead skin cells, and bacteria, then inflames beneath the skin’s surface. Typical triggers include hormonal surges, high‑glycemic diets, and chronic stress. Because the lesions are deep, they often leave lasting scars if left untreated.
Understanding Gut Health and the Microbiome
Gut health refers to the overall function of the digestive tract, especially the balance of microorganisms that live there. The gut microbiome comprises trillions of bacteria, fungi, and viruses that aid digestion, synthesize vitamins, and train the immune system. When this ecosystem stays diverse and stable, inflammation stays low and metabolism runs smoothly. Disruption-often called dysbiosis-can spill inflammatory molecules into the bloodstream, affecting organs far beyond the gut.
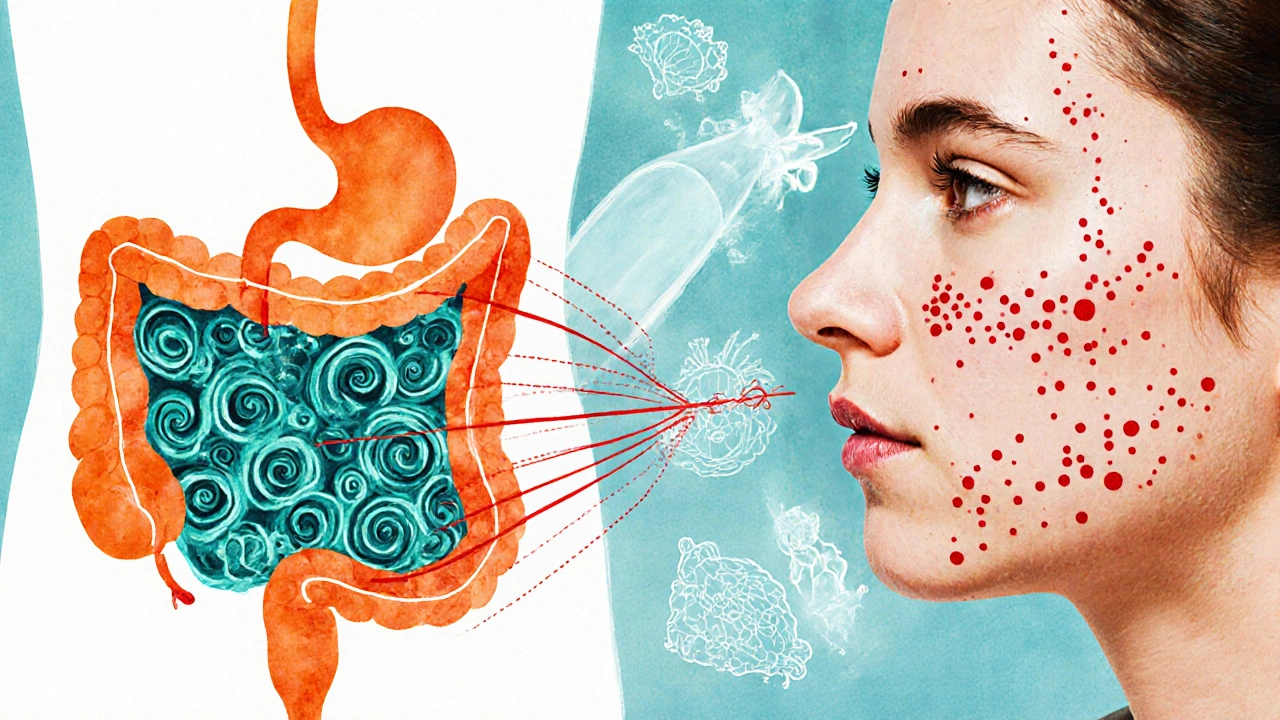
How the Gut Influences Skin: The Acne‑Gut Axis
The skin and gut share a two‑way communication channel called the gut‑skin axis. Here’s how it works:
- Bad gut bacteria produce endotoxins that cross the intestinal lining.
- These toxins trigger systemic inflammation, raising levels of cytokines like IL‑6 and TNF‑α.
- The immune system reacts by increasing oil production and plugging pores, setting the stage for hormonal imbalance and acne flare‑ups.
Researchers measuring blood markers in 2023 found that participants with severe acne had, on average, 35% higher C‑reactive protein-a sign of gut‑derived inflammation-than those with clear skin.
Key Gut‑Related Triggers for Nodular Acne
- Leaky gut: A compromised intestinal barrier lets undigested food particles and bacterial fragments enter the bloodstream, fueling inflammation.
- High‑sugar and refined‑carb diets: These feed harmful bacteria, cause rapid insulin spikes, and increase sebum production.
- Excessive alcohol or caffeine: Both can irritate the gut lining and alter microbiome composition.
- Chronic stress: Stress hormones lower gut motility and reduce beneficial bacterial counts.
- Antibiotic overuse: Broad‑spectrum antibiotics wipe out good microbes, often leading to a rebound overgrowth of acne‑promoting strains.
Food Choices That Support a Acne‑Friendly Gut
Eating for gut health doesn’t require a drastic overhaul, but certain foods consistently show benefits:
- Fermented foods: Sauerkraut, kimchi, kefir, and kombucha supply live probiotics that compete with acne‑linked bacteria.
- Prebiotic fibers: Foods like garlic, onions, bananas, and chicory root fuel good bacteria, helping them produce short‑chain fatty acids that calm inflammation.
- Omega‑3 rich fish: Salmon, mackerel, and sardines lower prostaglandin production, which can reduce oil gland activity.
- Low‑glycemic fruits and vegetables: Berries, leafy greens, and cruciferous veg keep insulin steady and reduce sebum spikes.
- Hydration: Plenty of water supports mucosal health and helps flush toxins.
Probiotics and Their Role in Managing Nodular Acne
Several clinical trials have tested probiotic supplementation specifically for acne. The most promising strains are:
| Strain | Typical Dose | Observed Skin Benefit | Key Study (Year) |
|---|---|---|---|
| Lactobacillus rhamnosus | 1×10⁹CFU/day | 20% reduction in nodule count after 12weeks | J. Dermatol. Sci., 2022 |
| Bifidobacterium breve | 5×10⁸CFU/day | Improved redness and lesion size | Int. J. Cosmet. Sci., 2021 |
| Streptococcus thermophilus | 2×10⁹CFU/day | Lowered serum IL‑6 by 15% | Clin. Exp. Dermatol., 2023 |
When choosing a supplement, look for a product that lists the strain name, dosage, and viability through the expiration date. Adding a probiotic alongside a high‑fiber diet gives the bacteria the fuel they need to colonize effectively.
Practical Steps to Reset Your Gut‑Skin Connection
- Audit your diet: Cut out refined sugars, processed snacks, and excessive dairy for at least four weeks. Replace them with the gut‑friendly foods listed above.
- Introduce fermented foods: Aim for a serving of kefir, kimchi, or yogurt daily. If you’re sensitive to dairy, opt for coconut yogurt with live cultures.
- Start a probiotic regimen: Choose one of the evidence‑backed strains, take it with a meal, and continue for a minimum of three months to see skin changes.
- Support gut lining: Include collagen peptides or bone broth, both rich in glutamine, which helps repair the intestinal barrier.
- Manage stress: Practice 10 minutes of mindful breathing or a short walk each day. Reduced cortisol correlates with lower gut permeability.
- Limit antibiotics: Only use them when prescribed, and follow up with probiotic support to restore balance.
Most readers notice a subtle reduction in redness within two weeks and a clearer complexion after eight to twelve weeks, provided they stay consistent.
When to Combine Gut‑Focused Strategies with Dermatology Treatments
Gut improvements can soften the severity of nodular acne, but deep‑seated nodules often need medical intervention. Consider these combinations:
- Topical retinoids + probiotic diet: Retinoids unclog pores while probiotics calm inflammation.
- Oral isotretinoin + gut‑protective nutrients: Supplement with omega‑3s and zinc to reduce the drug’s dryness side‑effects.
- Hormone‑modulating agents (e.g., spironolactone) + low‑glycemic meals: Stabilizes androgen spikes and reduces insulin spikes from carbs.
Always discuss any supplement changes with a dermatologist or GP to avoid interactions.
Common Pitfalls and How to Avoid Them
Even well‑meaning readers fall into traps that undo progress:
- Over‑supplementing: More than 10⁹CFU of a single strain can cause bloating; stick to tested doses.
- Chasing quick fixes: Skipping the diet overhaul and relying solely on pills rarely yields lasting results.
- Ignoring sleep: Poor sleep raises cortisol, which in turn impairs gut barrier function.
- Neglecting skin hygiene: Even with a perfect gut, using comedogenic lotions will re‑clog pores.
Future Directions: What Science Is Exploring
Emerging research in 2024‑2025 is looking at personalized microbiome transplants for acne, as well as bacteriophage therapy that specifically targets Cutibacterium acnes without harming beneficial gut microbes. While still experimental, these studies hint at a future where skin health can be tuned with a gut‑first approach.

Frequently Asked Questions
Can a gluten‑free diet improve nodular acne?
Gluten itself isn’t a direct acne trigger for most people, but many with gluten sensitivity also have leaky gut. Cutting gluten can reduce gut permeability, lower systemic inflammation, and sometimes lead to clearer skin. Test a 30‑day elimination to see if lesions improve.
How long does it take to see skin changes after starting probiotics?
Most clinical trials report noticeable reductions in redness and lesion count after 8‑12 weeks of consistent probiotic intake. Patience matters because gut bacteria need time to colonize and modulate the immune response.
Are there any probiotic foods that can worsen acne?
Fermented dairy like certain yogurts can be high in sugar or dairy fats, which may trigger acne in sensitive individuals. Choose low‑sugar, live‑culture options or non‑dairy alternatives to avoid this issue.
Is there a link between stress, gut health, and acne?
Yes. Stress elevates cortisol, which can increase gut permeability and shift the microbiome toward pro‑inflammatory species. Those changes raise systemic cytokines, which in turn boost oil production and inflammation in the skin.
Should I stop antibiotics if I’m on a probiotic plan for acne?
Never stop a prescribed antibiotic without consulting your doctor. However, you can start a probiotic within 2‑3 days of finishing the course, or use a probiotic‑rich yogurt during treatment to mitigate gut disruption.


michael Mc Laughlin
October 4, 2025 AT 01:12Thanks for the info its helpful.
Luke Schoknceht
October 4, 2025 AT 03:25The gut‑skin axis is a buzzword that has been stretched beyond its scientific limits. While there is emerging data linking dysbiosis to inflammatory pathways, the causal chain to nodular acne remains tenuous at best. Your risk calculator crudely aggregates diet, stress, and caffeine without accounting for individual microbiome diversity. Moreover, the probiotic strains listed are chosen more for marketability than for rigorously proven clinical outcomes. Lactobacillus rhamnosus, for instance, has shown modest benefits in mouse models, yet human trials are scarce and often confounded by diet. Bifidobacterium breve may improve redness, but the dosage you suggest is borderline ineffective for many adults. You also ignore the role of short‑chain fatty acids, which are pivotal in regulating sebaceous gland activity. Antibiotic exposure is indeed a risk factor, but the scoring system fails to differentiate between broad‑spectrum and narrow‑spectrum agents. Stress level is reduced to a single numeric input, overlooking cortisol’s circadian rhythm. Alcohol and caffeine are lumped together despite having distinct mechanisms that affect gut permeability. The calculator’s output is presented as a risk score, yet you provide no absolute risk figures or confidence intervals. This gives the false impression of precision where there is none. In practice, clinicians must consider dietary patterns, sleep hygiene, and topical treatments alongside any probiotic regimen. The interactive tool could benefit from a disclaimer about its exploratory nature. Finally, the UI’s aesthetic is pleasing, but functionality should not be sacrificed for style. Overall, readers should treat this as a conversation starter rather than a definitive diagnostic device.
mauricio gonzalez martinez
October 4, 2025 AT 05:38I feel like you left out the impact of fermented foods on inflammation.
Aakash Jadhav
October 4, 2025 AT 07:52Yo, the gut is like the backstage crew of a rock concert and the skin is the screaming crowd. If the crew messes up the amps, the crowd throws tomatoes, right? That's why we gotta keep those gut microbes humming. Think of probiotics as the VIP passes that let the good bugs get front‑row seats. So, if you're battling nodules, maybe it's time to upgrade your gut lineup.
Amanda Seech
October 4, 2025 AT 10:05I love the idea of connecting gut health to acne, but the info could be a bit clearer. Some of the terms are a little over my head, but I’m definetly excited to try probiotics. Hopefully it works!
Avinash Sinha
October 4, 2025 AT 12:18Behold, the saga of gut microbes battling the tyrannical oil glands! Our heroic Lactobacillus rides in on a CFU‑laden chariot, slashing nodule counts like a flamboyant swordsman. Meanwhile, Bifidobacterium whispers sweet nothings to the redness, calming it like a lullaby. And let us not forget Streptococcus, the silent guardian, reducing IL‑6 like a ninja in the night.
Geneva Angeles
October 4, 2025 AT 14:32Really appreciate the effort put into breaking down the gut‑skin connection. This kind of info can empower folks to look beyond just creams and pills. The probiotic suggestions are a solid starting point for anyone curious about inner health. It also reminds us that lifestyle tweaks can have ripple effects on our complexion. Keep the practical tips coming, they’re gold. Let’s all stay hopeful and keep experimenting responsibly.
Scott Shubitz
October 4, 2025 AT 16:45Your risk calculator is a glorified spreadsheet masquerading as science. Assigning arbitrary points to stress and coffee ignores the nuanced biochemistry at play. Even the probiotic doses you list are below therapeutic thresholds for most adults. If you truly want to help, provide peer‑reviewed references, not just glossy tables. Until then, consider this tool a marketing gimmick.
Soumen Bhowmic
October 4, 2025 AT 18:58Thanks for pointing out the probiotic strains, but I think we need to discuss prebiotic fibers too. Foods like chicory root, Jerusalem artichoke, and even bananas can feed the good bacteria and enhance their effect on skin health. Including these in the plan would make it more holistic. Also, a gradual introduction helps avoid gut upset. Overall, a balanced approach between diet and supplements is key.
Jenna Michel
October 4, 2025 AT 21:12Great breakdown! Integrating gut‑derived short‑chain fatty acids can modulate cutaneous inflammation via G‑protein coupled receptors. Consider adding a note on how butyrate‑producing strains influence sebum production. This mechanistic insight adds credibility and helps readers understand the why behind probiotic choices. Keep leveraging the latest microbiome research in future updates.
Abby Richards
October 4, 2025 AT 23:25Nice summary 👍. The emphasis on diet plus probiotics makes sense.
Lauren Taylor
October 5, 2025 AT 01:38I appreciate the inclusive tone of this discussion and the effort to make complex science accessible. By framing the gut‑skin connection as a collaborative journey, readers feel invited to experiment safely. The suggestion to monitor stress alongside dietary changes aligns with holistic health principles. It would be beneficial to add references to systematic reviews for those who wish to dive deeper. Overall, this post strikes a good balance between enthusiasm and evidence‑based guidance.
Vanessa Guimarães
October 5, 2025 AT 03:52While the optimism is commendable, the lack of rigorous data is alarming. One cannot simply prescribe probiotics without randomized controlled trials proving efficacy. Moreover, the tone borders on pseudo‑science, which may mislead vulnerable readers. A more skeptical, evidence‑first approach would be advisable.
Lee Llewellyn
October 5, 2025 AT 06:05Ah, the classic “let’s blame gut bacteria for everything” narrative. Sure, gut health matters, but turning it into a silver bullet for acne is a stretch. The calculator feels like a gimmick, ignoring genetics, hormonal fluctuations, and topical care. If you’re looking for a quick fix, you’ll be disappointed. Real solutions require a multifaceted strategy.
Drew Chislett
October 5, 2025 AT 08:18Interesting points about prebiotics. I wonder how different fiber sources compare in efficacy. Could be worth exploring in future posts.
Rajashree Varma
October 5, 2025 AT 10:32The philosophical angle of nurturing our internal ecosystem resonates deeply. By treating the gut as a community, we foster respect for its complexity. Precise dosing, as you noted, is essential to avoid dysbiosis. Encouraging mindful eating alongside supplementation creates a sustainable path to clearer skin.
Anshuman Pandey
October 5, 2025 AT 12:45I concur that short‑chain fatty acids act as signaling molecules influencing skin inflammation. Energy‑rich diets may skew microbial fermentation patterns, altering SCFA profiles. Therefore, aligning macro‑nutrient ratios with probiotic regimens could amplify benefits. Let’s keep encouraging interdisciplinary research.
Thomas Malloy
October 5, 2025 AT 14:58Cool discussion, thanks everyone.
Irene Harty
October 5, 2025 AT 17:12One must ask why pharmaceutical companies are silent on this gut‑skin paradigm. Their omission suggests a possible suppression of natural remedies. Proceed with caution and verify sources independently.
Jason Lancer
October 5, 2025 AT 19:25Another filler post, same old buzzwords. Nothing new here.