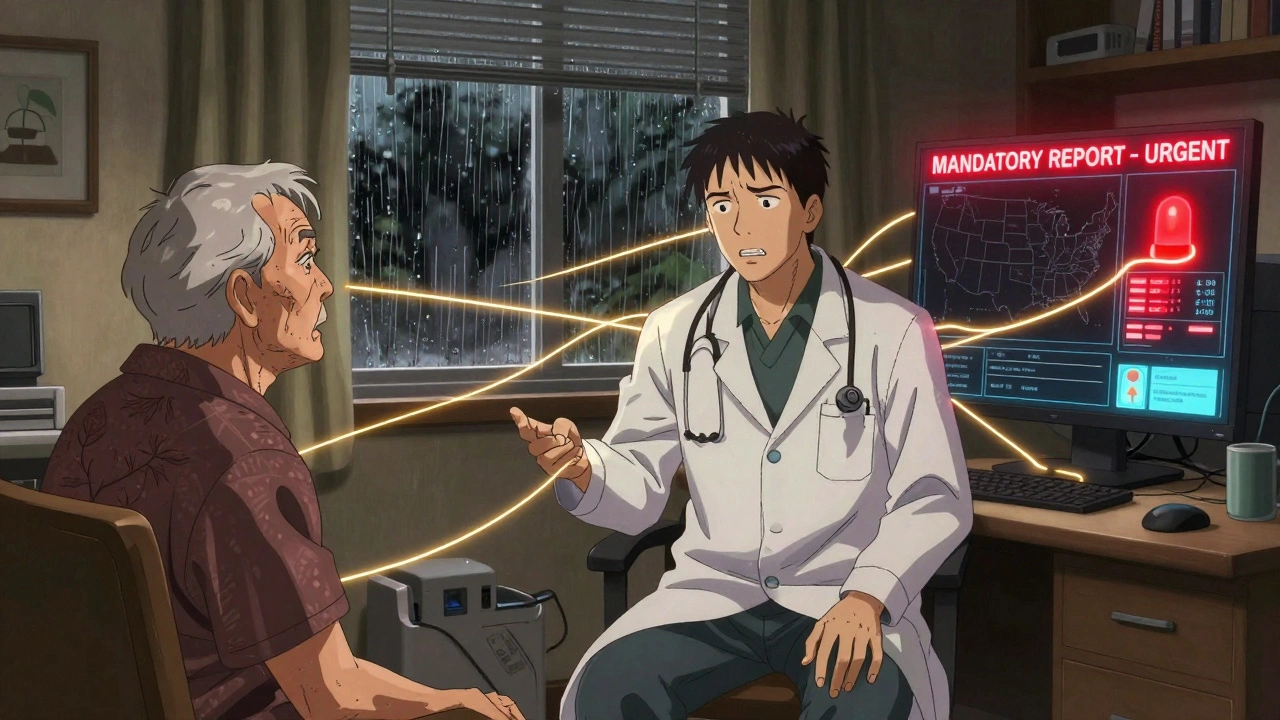
When a doctor sees a child with unexplained bruises, or a nurse notices an elderly patient with signs of neglect, they don’t just have a clinical concern-they have a legal duty to act. In the U.S., healthcare providers are not just caregivers; they’re also frontline reporters. Mandatory reporting laws require them to alert authorities when they suspect abuse, neglect, or public health threats. These rules aren’t optional. They’re written into state law, and failing to follow them can mean losing your license-or worse.
What You Must Report: The Big Four Categories
There are four main types of mandatory reporting that apply to most doctors and nurses. Each has its own rules, timelines, and consequences.- Child abuse and neglect: Required in all 50 states. You don’t need proof-just reasonable suspicion. That could mean unexplained injuries, behavioral changes, or a child who flinches at touch.
- Elder and vulnerable adult abuse: 47 states and D.C. require reporting. This includes physical harm, financial exploitation, or being left without food, medicine, or hygiene care.
- Public health threats: 57 diseases are nationally notifiable. Think tuberculosis, measles, or syphilis. Some, like anthrax, must be reported within an hour. Others, like Lyme disease, have a 7-day window.
- Professional misconduct: If you see a colleague prescribing illegally, practicing while impaired, or falsifying records, you’re often required to report them. This isn’t gossip-it’s patient safety.
These aren’t suggestions. They’re legal obligations. And the penalties for ignoring them are real. In 2021, 12% of malpractice claims against physicians involved failure to report. That’s not a small risk.
Timing Matters: How Fast Do You Have to Act?
The clock starts ticking the moment you suspect something. But the deadline? It varies wildly by state and type of case.For child abuse:
- In California, Texas, and Florida, you must report immediately-usually within 24 hours.
- In Minnesota and Michigan, you have up to 48 hours.
- In some states, you can call first, then submit written reports later.
Elder abuse reporting is even more confusing. Only 14 states require all healthcare workers to report it. In Texas, you’re not legally required to report elder abuse unless you work in a nursing home. In New York, you must report domestic violence. In Utah, you’re protected by law if you report-no retaliation allowed.
Public health reports are mostly automated now. Hospitals use electronic systems that send data directly to state health departments. That cuts reporting time from 30 minutes to under 5. But if you’re in a small clinic without that tech, you’re still on the hook to file by phone or form.
What Information Goes in the Report?
A good report isn’t just a hunch. It needs facts. Each state has its own checklist, but most require:- Name, age, and address of the victim
- Name and contact info of the caregiver or suspect
- Description of the injury, behavior, or condition
- When and how you noticed it
- Your name and license number (as the reporter)
Miss one piece? Your report might be rejected. In Michigan, a nurse once lost her case because she didn’t include the child’s school name. In California, a doctor’s report was flagged because he wrote “possible abuse” instead of describing the bruise pattern.
Documentation is your armor. Write down exactly what you saw, heard, and did. Date it. Sign it. Keep a copy. If you’re ever questioned later, your notes are your proof you did your job.
The Ethical Tightrope: Confidentiality vs. Safety
HIPAA protects patient privacy. But mandatory reporting is one of the few exceptions. You’re legally allowed-and sometimes required-to break confidentiality.That creates tension. A 2020 AMA survey found 68% of physicians say patients withhold critical information because they fear reporting. One pediatrician shared on Reddit: “A teen came in for depression. When I mentioned child services, she stopped coming. She said she’d rather suffer than be taken away.”
But the other side matters too. In Michigan, a nurse reported a father who was starving his 3-year-old. Investigators found the child was also being locked in a closet. That report saved her life.
The ethical question isn’t whether to report-it’s how to do it without destroying trust. The best approach? Be transparent. Say: “I’m required by law to report certain things if I think someone’s in danger. I’m not accusing you-I’m trying to get help.”
Reporting a Colleague: The Hardest Call
Reporting a fellow nurse or doctor feels like betrayal. You work side by side. You’ve shared meals, shifts, and trauma.But if a colleague is drunk on shift, forging prescriptions, or ignoring infection control, you’re putting patients at risk. And the law says you must report it.
Minnesota requires Chief Nursing Executives to report nurse misconduct within 30 days. Nebraska has the same rule. But individual nurses? They’re often allowed-but not required-to report. That’s a gap.
One nurse in Utah reported unsafe staffing levels. Despite state laws protecting reporters, she was demoted two weeks later. She filed a complaint and won-but it took 11 months. That’s the cost of doing the right thing.
Here’s what helps: use your institution’s formal reporting system. Don’t whisper it to a friend. Document everything. Go through the chain of command. If your hospital has a whistleblower hotline, use it. And know your rights: 18 states have laws that protect reporters from retaliation.
Telehealth and the State Law Maze
If you’re a telehealth provider, you’re probably reporting across state lines. That’s a legal minefield.A 2022 study found 42% of telehealth providers were confused about which state’s laws applied. One doctor in California treated a child living in Arizona. He reported the abuse to California. But Arizona’s law required the report to be filed by the Arizona provider. The child’s case stalled for months.
Best practice? Always report to the state where the patient is located. If you’re unsure, call your state’s reporting hotline. Some states, like Washington, offer 24/7 support. Others? You’re on your own.

How to Stay Compliant
You don’t need to memorize 50 state laws. But you do need a system:- Get trained. Most hospitals require annual mandatory reporting training. Don’t skip it.
- Know your state’s website. Search “[Your State] mandatory reporting healthcare.” Most have PDF guides and hotline numbers.
- Keep a quick-reference sheet on your desk or phone. List the top 3 reportable conditions and who to call.
- Use your hospital’s reporting portal. Many now have one-click systems for child, elder, and public health reports.
- When in doubt, report. It’s better to file a report that turns out to be unnecessary than to miss one that could save a life.
And remember: you’re not alone. Every state has a child protective services line, an adult protective services line, and a public health hotline. Use them. Ask questions. No one expects you to be a legal expert-but they do expect you to try.
What’s Changing in 2025
The system is slowly getting smarter. By 2025, the federal government plans to roll out a nationwide electronic reporting system for public health data. That means fewer phone calls, fewer missed reports.AI tools are also being tested. At Massachusetts General Hospital, a pilot program used AI to flag potential abuse cases in patient notes. It cut reporting errors by 38%. That’s not replacing you-it’s helping you.
But the biggest change? More states are adding human trafficking as a reportable condition. That’s new. And it’s growing fast. By 2022, 18 states had added it. More will follow.
Final Thought: You’re the First Line
You see things no one else does. A child who won’t make eye contact. An elderly woman with a missing tooth and a trembling hand. A nurse who’s been drinking before shift. You don’t need to solve it. You just need to report it.The system isn’t perfect. It’s messy. It’s inconsistent. But it works. A 2019 JAMA study found states with mandatory reporting identified 37% more child abuse cases than those without.
So when you’re tired, overwhelmed, or scared-remember: your report might be the only thing standing between a child and harm. Or between a patient and a dangerous provider. Or between a community and an outbreak.
You’re not just a nurse or a doctor. You’re a protector. And that’s a responsibility you can’t afford to ignore.
Do I have to report if I’m not 100% sure?
Yes. Mandatory reporting is based on "reasonable suspicion," not proof. If something feels wrong-unexplained injuries, sudden behavioral changes, inconsistent stories-you report it. The authorities will investigate. You’re not expected to be a detective.
Can I get in trouble for reporting too much?
No. As long as you report in good faith, you’re protected from civil or criminal liability in all 50 states. Even if your report turns out to be wrong, you won’t be punished. But if you fail to report when you should, you could lose your license or face fines.
What if my hospital doesn’t train me on reporting?
You’re still legally responsible. Training is required by law in most states, but if your employer skips it, you need to find the info yourself. Search your state’s Department of Health website. Many offer free online modules. The Child Welfare Information Gateway also has free training for mandatory reporters.
Can I report anonymously?
In most cases, no. You must provide your name and license number. This protects against false reports and allows investigators to follow up. But your identity is confidential-only authorized personnel can access it. You won’t be publicly named.
What if I report a colleague and they get fired?
If your report was honest and based on facts, you’re protected under whistleblower laws in 18 states. But if your colleague is fired because of your report, that doesn’t mean you did something wrong-it means the system worked. Your job is to protect patients, not to protect coworkers from consequences.
Do I need to report if the patient says they don’t want me to?
Yes. Patient consent doesn’t override mandatory reporting laws. If a child is being abused, or an elderly person is being exploited, their wishes don’t change your legal duty. Explain this to them calmly: "I care about you, but I’m required by law to report this to keep you safe."


Doris Lee
December 10, 2025 AT 13:09Just wanted to say thank you for writing this. So many of us feel overwhelmed by the legal maze, but you made it feel manageable. You’re right-we’re not detectives, we’re the first pair of eyes that might save someone.
Michaux Hyatt
December 11, 2025 AT 06:18Had a case last month where a teen came in with bruising she said was from ‘falling down the stairs.’ Didn’t have proof, but the pattern? Classic. Filed the report. Got a call two days later-the mom had been arrested. Kids don’t always tell us the truth. We have to be the ones who see it anyway.
Queenie Chan
December 12, 2025 AT 07:58God, I love how this post doesn’t sugarcoat it. You know what’s wild? The fact that in some states, you can report elder abuse with a text message. In others, you need a notarized form and a witness. It’s like healthcare’s version of Dungeons & Dragons-except the dragon is paperwork and the treasure is avoiding a lawsuit.
I once spent 45 minutes on the phone with a state hotline because the nurse before me forgot to include the patient’s middle name. The woman on the line didn’t even blink. Said, ‘Happens every Tuesday.’
And AI flagging abuse in notes? That’s not the future-that’s already here. My hospital’s system auto-tags phrases like ‘afraid to go home’ or ‘doesn’t eat with family.’ It’s creepy. But also… kinda genius?
Also, can we talk about how telehealth is a legal nightmare? I treated a kid in Idaho from Oregon. Reported to Oregon. Idaho said, ‘Not our problem.’ Now the kid’s in limbo. No one’s responsible. No one’s accountable. Just a bunch of state lines and silence.
And yes-I’ve reported colleagues. One was giving insulin to non-diabetic patients because ‘they looked tired.’ I didn’t sleep for three nights after. But I slept better knowing I didn’t let it slide.
Regan Mears
December 12, 2025 AT 15:05Thank you for this. I’m a new RN, and I was terrified to report a suspected case last week-I kept thinking, ‘What if I’m wrong?’ But you’re right: it’s not about being right. It’s about being brave enough to speak up. I called CPS. They said, ‘We’re glad you did.’ That’s all I needed to hear.
Also, I write everything down. Every word. Every pause. Every sigh. I keep a little notebook in my scrubs pocket. If I’m ever questioned, I’ve got the truth right there. No guesswork. No ‘I think.’ Just facts.
And yes-I’ve had patients cry and beg me not to report. I say, ‘I’m not here to punish you. I’m here to make sure you’re safe.’ Sometimes they don’t believe me. But I keep saying it anyway.
David Palmer
December 13, 2025 AT 03:08Bro, I just work the night shift. I don’t wanna be a cop. Why do I gotta be the one to report everything? I just wanna get through my shift without crying.
Frank Nouwens
December 14, 2025 AT 06:29While I appreciate the intent of this piece, I must emphasize the procedural inconsistencies across jurisdictions. The absence of a federally standardized reporting protocol introduces systemic inefficiencies and potential legal vulnerabilities. For example, the variance in reporting windows for elder abuse-from immediate to nonexistent-undermines the very principle of universal protection. A unified, digitized, real-time reporting architecture is not merely desirable-it is ethically imperative.
Neelam Kumari
December 16, 2025 AT 04:04Oh wow. So now nurses are secret police? Next thing you know, we’ll be reporting people for ‘suspicious eye contact’ or ‘too much smiling.’
And let’s be real-most of these reports are just nurses being dramatic. ‘He didn’t hold the door open for me!’-oh no, child abuse!
At least in India, we don’t have this nonsense. People take care of their own. No government telling you who to rat out.
Nikki Smellie
December 17, 2025 AT 07:29Have you considered that mandatory reporting is a Trojan Horse for the Deep State to monitor families? The moment you report, your patient’s data is fed into a federal algorithm that flags ‘high-risk households.’ That’s how they know who to surveil. And the ‘protected identity’? It’s a lie. They track your IP, your license number, your hospital login. This isn’t safety-it’s social control. And the AI? It’s learning your biases. It’s already been proven to flag Black children 3x more often. You’re not helping. You’re enabling.
Also, I’ve seen the reports. They’re full of typos. And the hotline? It’s always busy. So you’re wasting your time. And your soul.
Kaitlynn nail
December 19, 2025 AT 02:32So… we’re the moral compasses now? Cool. I’ll just go sit in a lotus position and chant ‘I am the law’ while I file this report.