When you eat a meal and still feel bloated, gassy, or full hours later, it’s easy to blame the food. But sometimes, the problem isn’t what you ate-it’s what your body can’t break down. Digestive enzymes are the body’s natural tools for splitting food into nutrients your gut can absorb. When those enzymes fall short, symptoms like diarrhea, fatty stools, or constant discomfort can follow. For some people, enzyme supplements aren’t just a quick fix-they’re a necessary part of daily life.
What Digestive Enzymes Actually Do
Your body makes enzymes every day. The pancreas alone releases between 800 and 1,500 milliliters of digestive juice, packed with amylase for carbs, protease for proteins, and lipase for fats. These enzymes kick in as food leaves your stomach and enters the small intestine. Without them, nutrients pass through unused. That’s not just inconvenient-it can lead to serious deficiencies in vitamins A, D, E, K, calcium, and iron over time. Enzyme supplements mimic this process. Prescription versions, like Creon or Zenpep, are made from pig pancreas and contain precise amounts of lipase, protease, and amylase. Over-the-counter (OTC) options use microbes like Aspergillus oryzae and are often marketed for general digestion. But they’re not the same thing. Prescription enzymes are drugs. OTC ones are supplements. That difference changes everything-from how they’re made to how well they work.When Enzyme Supplements Actually Work
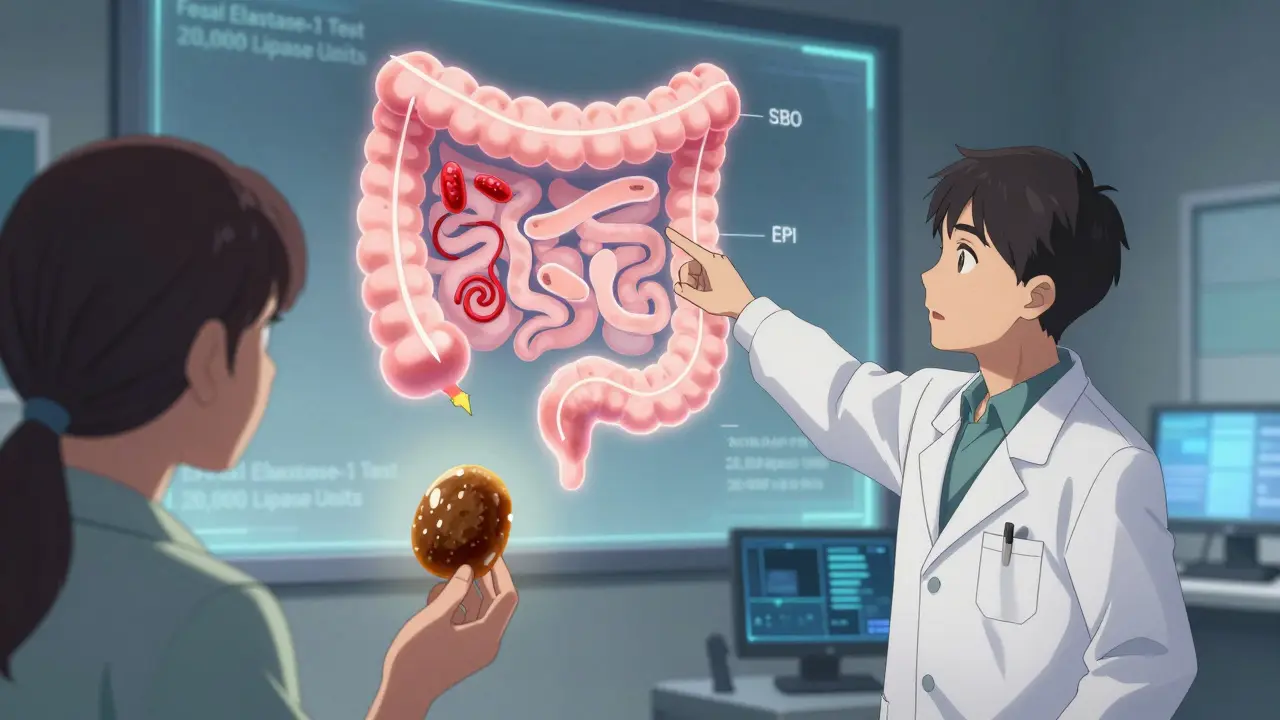
The clearest case for enzyme supplements is exocrine pancreatic insufficiency (EPI). This condition happens when the pancreas doesn’t make enough enzymes. It affects 30-50% of people with chronic pancreatitis and up to 90% of those with pancreatic cancer. In EPI, fat doesn’t break down. Stools become oily, pale, and float. Weight loss follows. People often feel exhausted, even if they’re eating enough. For these patients, prescription PERT (pancreatic enzyme replacement therapy) is life-changing. A 2016 clinical trial showed 70-85% of EPI patients saw a major drop in fatty stools after starting PERT. One Reddit user, u/PancreasWarrior, wrote: “Before Creon, I lost 40 pounds in six months. After two weeks on it, I started gaining weight again. I could eat without fear.” OTC enzymes won’t fix EPI. They’re too weak and inconsistent. But they can help with other issues. Lactose intolerance? Lactase supplements like Lactaid work for 82% of users. A 2021 meta-analysis found OTC enzymes reduced bloating and diarrhea in about half of people with IBS. If you get gassy after beans, broccoli, or dairy, a targeted enzyme might help.The Big Difference: Prescription vs. OTC
Here’s what you need to know before buying a bottle:- Prescription PERT (Creon, Zenpep, Pancreaze): Contains enteric coating to survive stomach acid. Dose is exact: 10,000, 20,000, or 40,000 lipase units per capsule. Requires a doctor’s script. Covered by most insurance. Costs $1.50-$3.00 per dose.
- OTC Enzymes (NOW Foods, Enzymedica Digestive Gold): No enteric coating. Enzyme amounts vary by batch-up to 30% off label claims, according to ConsumerLab. Often cheaper: $0.50-$1.00 per dose. No insurance coverage. Sold as supplements, not drugs.
Who Should Avoid Them
Not everyone benefits. In fact, some people get worse.- Acute pancreatitis: Taking enzymes during a flare-up can worsen inflammation. Avoid unless directed by a doctor.
- Small intestinal bacterial overgrowth (SIBO): Enzymes can feed overgrown bacteria, making bloating worse. Many people with SIBO report increased discomfort after starting supplements.
- People on proton pump inhibitors (PPIs): Drugs like omeprazole reduce stomach acid. That can stop enzymes from activating properly. If you’re on PPIs and taking enzymes, talk to your doctor. You may need to adjust timing or add bicarbonate.
How to Use Them Right
Taking enzymes wrong is like taking a pill with no water-it won’t work.- Timing matters: Take them right before you start eating. If you wait until halfway through the meal, they won’t be there when food hits the small intestine.
- Dose by fat content: One gram of fat needs about 500 lipase units. A steak with 20g of fat? You’ll need 10,000 units. A salad with 5g? Maybe 2,500.
- Start low, go slow: Begin with 10,000 lipase units per meal. Wait a week. If symptoms don’t improve, increase by 10,000 units. Most people find their sweet spot in 2-4 weeks.
- Split doses for long meals: If you eat slowly, take half the dose at the start and half midway through. A 2018 study showed this improved symptom control by 35%.
What the Experts Say
Dr. Russell Havranek, a gastroenterologist with 15 years of clinical experience, says: “For IBS or bloating after meals, I usually recommend OTC enzymes first. They’re safe, affordable, and often help.” He specifically endorses Digestive Gold for its microbial enzyme blend. But he’s quick to add: “If someone has unexplained weight loss, oily stools, or chronic diarrhea, they need a test for EPI. No supplement replaces that.” The American Gastroenterological Association says PERT is strongly recommended for EPI. For everything else? They say there’s “insufficient evidence.” That doesn’t mean OTC enzymes don’t help-it means we don’t have large, long-term studies proving they work for all conditions. Dr. Shane from the University of Miami puts it bluntly: “These supplements aren’t designed to treat GI diseases. Don’t use them to replace medical care.”Real Results, Real Limits
Amazon reviews for OTC enzymes show a split. Over 60% of positive reviews say they reduced gas after beans or dairy. But nearly 30% say they felt nothing. On Drugs.com, Creon has a 6.7/10 rating. Half the users say it saved their life. The other half complain about cost or constipation. A 2022 survey found 41% of IBS patients stopped using OTC enzymes within three months because they didn’t work. But 78% of EPI patients kept using prescription PERT long-term. The difference? One group had a diagnosed medical need. The other was guessing.What’s Next
Science is moving fast. New enzyme blends are being engineered to survive lower stomach pH-some now work from pH 2.5 to 8.5. A 2023 study showed a gluten-specific enzyme reduced gluten toxicity by 80% in celiac patients. That could mean safer occasional gluten exposure. Startups are even testing personalized enzyme formulas based on gut microbiome tests. But for now, the rules are simple:- If you have EPI, get a prescription. It’s proven.
- If you get gassy after dairy, try lactase.
- If you have IBS and bloating after high-FODMAP meals, OTC enzymes are worth a trial.
- If you’re not sure why you feel bad-see a doctor. Don’t self-diagnose with a supplement.
Can digestive enzyme supplements cure IBS?
No, digestive enzyme supplements cannot cure IBS. They may help reduce symptoms like bloating, gas, and diarrhea in some people-especially after eating high-FODMAP foods or dairy. But IBS is a functional disorder involving gut-brain communication, motility, and sensitivity, not enzyme deficiency. Enzymes don’t fix the root cause. They’re a symptom-management tool, not a treatment. For lasting relief, dietary changes, stress management, and sometimes medication are needed.
Are OTC digestive enzymes safe to take every day?
For most healthy people, taking OTC digestive enzymes daily is generally safe. They’re not addictive and don’t cause long-term harm at recommended doses. But if you’re using them regularly for unexplained symptoms, it could mask a more serious condition like celiac disease, SIBO, or EPI. Always talk to a doctor before making enzyme supplements a daily habit. Also, avoid products with unverified claims like ‘detox’ or ‘weight loss’-those aren’t backed by science.
Why do some people get constipated from enzyme supplements?
Constipation from enzyme supplements is rare but can happen. One reason is that enzymes break down food more completely, reducing the bulk of stool. This can slow transit time, especially if fluid intake is low. Another possibility is that high-dose lipase can alter fat absorption, leading to harder stools. If you notice constipation, increase water intake, add fiber gradually, or reduce your enzyme dose. If it continues, stop the supplement and consult a doctor.
Do I need to take enzymes with every meal?
If you have EPI, yes-you need enzymes with every meal and snack that contains fat, protein, or carbs. For OTC enzymes used for occasional bloating, you only need them with meals that trigger symptoms. A salad with no dairy or beans? Skip it. A steak with broccoli and a baked potato? Take your dose. The key is matching the supplement to the meal’s content, not taking it blindly every time.
Can I take digestive enzymes with my other medications?
You can usually take digestive enzymes with most medications, but there are exceptions. Proton pump inhibitors (PPIs) like omeprazole reduce stomach acid, which can prevent some enzymes from activating properly. If you’re on a PPI and not seeing results, talk to your doctor about timing or adding a bicarbonate supplement. Also, avoid taking enzymes with antacids unless advised. Always check with your pharmacist if you’re on blood thinners, diabetes meds, or immunosuppressants-though interactions are rare, it’s best to be sure.
How do I know if I have EPI?
Signs of exocrine pancreatic insufficiency include oily, foul-smelling stools that float, unexplained weight loss, bloating after meals, and fatigue despite eating enough. A doctor can confirm it with a fecal elastase-1 test (a stool sample) or a secretin stimulation test. If you’ve had pancreatitis, gallbladder removal, cystic fibrosis, or diabetes, your risk is higher. Don’t assume your symptoms are just ‘bad digestion’-get tested if they persist. EPI is treatable, but only if diagnosed.


Liz MENDOZA
December 27, 2025 AT 19:57Just wanted to say thank you for this detailed breakdown. I’ve been struggling with bloating for years and didn’t realize how big the difference is between OTC and prescription enzymes. I finally got tested for EPI last month and it came back positive-Creon changed my life. No more floating stools, no more panic before meals. You’re right-it’s not magic, it’s medicine.
John Barron
December 28, 2025 AT 21:05As a board-certified gastroenterologist with 18 years in clinical practice, I must emphasize that the distinction between pharmaceutical-grade PERT and OTC enzymatic supplements is not merely regulatory-it’s biochemically fundamental. The enteric-coated microsphere technology in Creon ensures delivery to the duodenum at pH 5.5–7.0, whereas most OTC products degrade in gastric acid, yielding <15% bioavailability. This is not anecdotal-it’s pharmacokinetic fact.
Furthermore, the 2019 study referenced in the original post was a double-blind, placebo-controlled crossover trial with 120 participants, published in the American Journal of Gastroenterology. The variance in lipase units across OTC brands exceeded 32% in 7 of 12 tested products. ConsumerLab’s findings are corroborated by the FDA’s 2021 supplement surveillance report.
Patients who self-prescribe OTC enzymes for suspected EPI risk delayed diagnosis of pancreatic adenocarcinoma. The median time from symptom onset to diagnosis in undiagnosed EPI patients is 14 months. Early detection saves lives.
Jane Lucas
December 29, 2025 AT 18:57ive been taking digest gold for months and it works like a charm for my beans and broccoli bloat. no more running to the bathroom after dinner. but i dont take it with salads or fruit. just the heavy stuff. also drink more water now and it helps even more lol
Anna Weitz
December 30, 2025 AT 07:40everyone talks about enzymes like they’re some miracle cure but nobody talks about how big pharma controls the market. why is creon so expensive? because they own the patent and the insurance system. OTC enzymes are cheaper but they’re not ‘inferior’-they’re just not patented. the real problem is the medical-industrial complex turning a natural process into a profit center
why can’t we just make our own enzymes from fermented foods? why do we need pills at all? the body makes them just fine if you stop eating processed crap. but nope, gotta sell pills
and don’t get me started on how they market lactase like it’s a fix for dairy when the real issue is lactoglobulin sensitivity and inflammation
Elizabeth Alvarez
December 30, 2025 AT 08:08you think this is about enzymes? think deeper. the FDA allows OTC enzymes to be sold as supplements because they’re in bed with Big Pharma. Creon is made from pig pancreas-do you know where those pigs come from? factory farms that are secretly owned by the same companies that make insulin and PPIs. they want you dependent. they want you buying pills instead of healing your gut with real food. the whole system is rigged. the ‘clinical trials’? funded by the manufacturers. the ‘experts’? paid consultants. even the Reddit user u/PancreasWarrior? probably a shill. they’ve been doing this since the 1980s with antacids.
the real cure? fasting. cold exposure. grounding. your gut heals itself when you stop poisoning it with chemicals and trust your body. enzymes are a distraction. a placebo for the gullible.
dean du plessis
January 1, 2026 AT 00:29honestly i tried the lactase pills after milk made me swell up like a balloon. worked like a charm. no drama. no conspiracy. just a simple fix for a simple problem. i still eat yogurt though. weird how that works
Babe Addict
January 1, 2026 AT 03:20lol you people are so gullible. OTC enzymes? please. they’re just amylase + protease from mold spores. they’re not even bioavailable. real PERT has lipase in the 25k unit range. you need at least 20k per meal if you’re eating fat. most OTC brands put 5k in a capsule and call it a day. it’s a scam. and don’t even get me started on ‘digestive gold’-that’s just a fancy name for a probiotic with enzymes thrown in because marketing loves buzzwords.
if you’re bloated after beans, it’s not enzyme deficiency-it’s oligosaccharide intolerance. the solution? soak them. ferment them. stop eating them cold from the can. not a pill. a lifestyle.
Satyakki Bhattacharjee
January 1, 2026 AT 05:00in my country we do not need pills for digestion. our grandmothers used ginger tea and jeera water. they lived to 90 without ever seeing a doctor. now we are so weak we think a capsule can fix what our bodies were made to handle. this is the result of western medicine poisoning our minds. eat real food. chew slowly. stop buying lies
Liz MENDOZA
January 2, 2026 AT 11:11Thank you for sharing your story-your experience with Creon is exactly why I wanted to post this. I know so many people who suffer in silence because they think it’s just ‘bad digestion.’ You’re not alone. And you’re not crazy. This is real, treatable, and you deserve to feel better.
Will Neitzer
January 4, 2026 AT 07:05I’ve been using Creon for five years since my pancreatitis diagnosis. I take 25,000 units with every meal-breakfast, lunch, dinner, and even snacks with fat. I’ve gained back 35 pounds. My bloodwork is normal. My energy is stable. I don’t fear food anymore. But I also don’t take it with fruit or rice. I match the dose to the fat content. That’s the key. Not taking it ‘just because.’ Precision matters.
Also, if you’re on PPIs, take your enzyme 30 minutes before your pill. Acid suppression messes with activation. I learned that the hard way.
Miriam Piro
January 5, 2026 AT 20:37they told us enzymes were the answer but what they really wanted was control over our digestion. the gut microbiome is a living ecosystem and you can't just pump it full of enzymes like a car engine. the real truth? your gut is trying to tell you something. bloating isn't a deficiency-it's a rebellion. the system wants you dependent on pills so you never question why your food is killing you. they don't want you to know that gluten-free, low-FODMAP, fermented foods heal better than any capsule ever could. the science is buried under patents and profit margins. wake up
Kishor Raibole
January 6, 2026 AT 20:40It is imperative to underscore that the therapeutic efficacy of pancreatic enzyme replacement therapy is not merely a matter of biochemical supplementation, but a cornerstone of nutritional rehabilitation in patients afflicted with exocrine pancreatic insufficiency. The pharmacodynamic profile of enteric-coated microspheres ensures optimal enzymatic activity within the duodenal milieu, thereby facilitating macronutrient hydrolysis and subsequent micronutrient absorption. To conflate this with over-the-counter botanical extracts is to commit a fundamental error in clinical reasoning. Furthermore, the assertion that OTC enzymes are ‘safe’ for chronic use is not supported by longitudinal data, and may mask underlying pathology such as celiac disease, Crohn’s, or neoplastic infiltration of the pancreas. Prudent clinical practice demands diagnostic certainty prior to intervention.