Why so many people still don’t trust generic drugs
Most people don’t realize that nearly 9 out of 10 prescriptions filled in the U.S. are for generic drugs. Yet, if you ask a patient if they’d take a generic instead of a brand-name pill, many still say no. Why? Because they think generics are weaker, less safe, or made in cheaper factories. The truth? The FDA requires generic drugs to match brand-name drugs in every way that matters-active ingredient, strength, how fast they work, and how well they work in the body. But that message isn’t getting through.
What the FDA says about generic drugs
The U.S. Food and Drug Administration (FDA) doesn’t just approve generic drugs-it tests them. Every single one. To get approval, a generic must prove it delivers the same amount of active medicine into the bloodstream as the brand-name version, within a strict range of 80% to 125%. That’s not a guess. It’s measured in clinical studies using blood tests that track how the drug moves through the body. This isn’t new. The FDA has been doing this for over 40 years. And in that time, no credible study has shown generics to be less effective than brand-name drugs for the vast majority of conditions.
There are over 2,100 free educational resources on the FDA’s website-videos, infographics, fact sheets-all in English and Spanish. These aren’t marketing materials. They’re plain-language tools designed for community health workers, pharmacists, and patients to use in conversations. One simple message repeats across them all: generic drugs work the same.
The money-saving power of generics
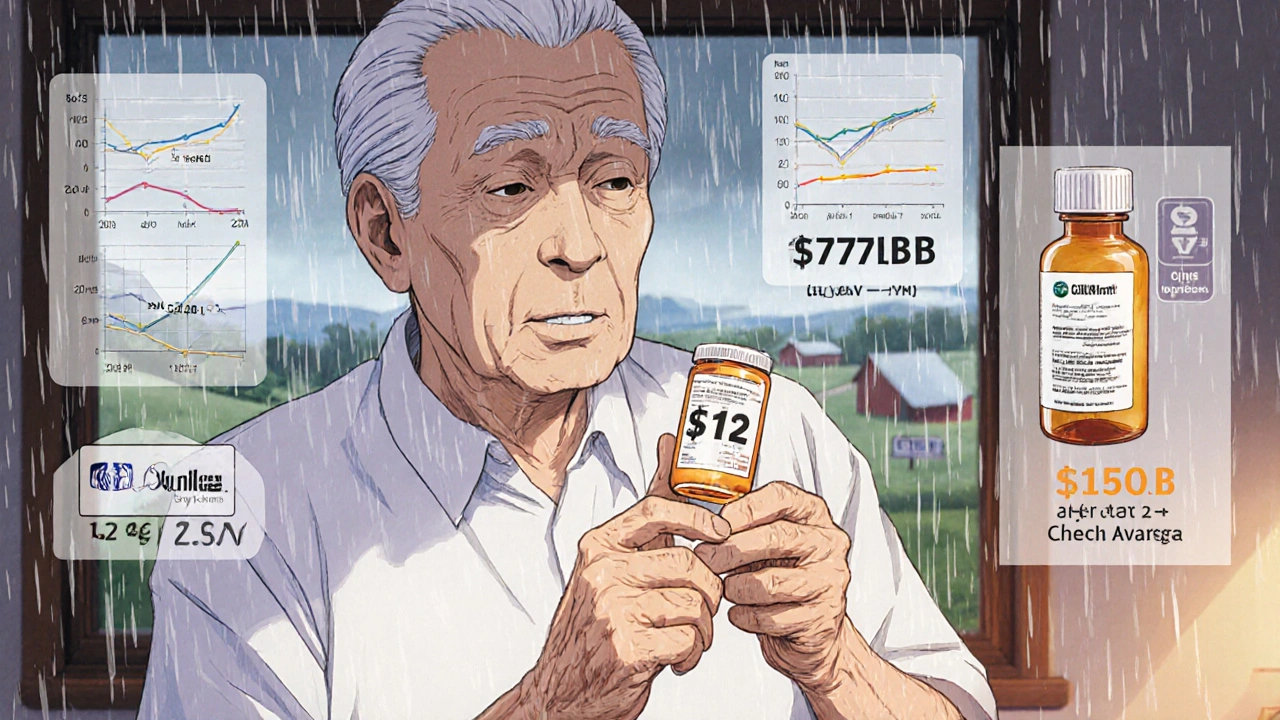
Generic drugs cost 80% to 85% less than their brand-name counterparts. That’s not a small difference. It’s life-changing for people on fixed incomes, those without good insurance, or families juggling multiple prescriptions. In 2022 alone, generics saved the U.S. healthcare system $377 billion. That’s enough to cover the cost of insulin for every diabetic in the country for over a year.
Imagine a patient taking a blood pressure pill that costs $150 a month as a brand name. Switching to the generic? It drops to $12. That’s not a luxury-it’s a necessity. When people can’t afford their meds, they skip doses. When they skip doses, their health gets worse. Generics help break that cycle.
Why patients still hesitate-even when doctors recommend generics
Here’s the surprising part: even when doctors say, “This generic is just as good,” many patients still say no. Why? Because of how the pills look. A blue oval pill becomes a white circle. A red capsule turns into a green one. Patients think, “This isn’t the same.”
A 2022 University of Michigan study found that 23% of patients questioned whether their medication worked after switching to a generic-just because the shape or color changed. That’s not about science. It’s about perception. And it’s something community health workers can fix.
One proven method? The “Teach-Back” technique. Instead of saying, “This is a generic,” say: “The FDA says this pill has the exact same medicine as your old one, in the same amount, and it works the same way. Can you tell me back what that means to you?” When patients repeat the key points in their own words, understanding sticks. Community Health Center of Burlington used this method in 2021 and saw patient acceptance of generics jump by 37% in just six months.
When generics don’t work-rare exceptions and real concerns
There are a few areas where switching generics causes problems. The most talked-about is epilepsy. A 2023 study in Epilepsy & Behavior found that when patients switched between different generic versions of antiseizure drugs, a small number had more seizures. But here’s the full picture: the American Academy of Neurology says this is an extremely rare exception. The problem isn’t that generics are inferior-it’s that switching between multiple generic brands can cause tiny differences in how the body absorbs the drug. For patients with tightly controlled conditions like epilepsy, staying on the same generic brand matters.
That’s why doctors who treat epilepsy often write “dispense as written” on prescriptions. It’s not about distrust in generics. It’s about consistency. For 95% of other conditions-diabetes, high cholesterol, asthma, depression-switching generics is completely safe and effective.
The nocebo effect: believing you’ll feel worse makes you feel worse
There’s a powerful psychological trick at play. It’s called the nocebo effect. When patients are told, “This is a generic,” they’re more likely to report side effects-even if they’re taking the exact same pill they took before, just in a different package.
A 2021 study in the Annals of Internal Medicine showed that when patients were told they were getting a generic, 18.7% more of them stopped taking the drug because they thought it wasn’t working. But when they took the same pill without knowing it was generic, they didn’t report more side effects. The medicine didn’t change. Their belief did.
Community health presentations can help by changing the language. Instead of saying, “This is a cheaper option,” say, “This is the same medicine, approved by the FDA, and it’s helping millions save money without losing effectiveness.”
Who’s winning with generics-and who’s being left behind
Generics are used in 93% of urban areas. In rural areas? Only 78%. Why? Fewer pharmacists. Less access to education. Longer distances to clinics. People in rural communities are more likely to be older, on fixed incomes, and managing multiple chronic conditions. They need generics the most-and they’re getting them the least.
That’s changing. The FDA’s 2022 report on health equity showed that switching to generics improved medication adherence by 22% among low-income patients. That’s why the National Association of Community Health Centers now requires all patient counseling sessions to include generic drug education. Starting in 2024, every community health center must teach patients why generics are safe, effective, and affordable.
Medicare Part D plans are also stepping up. By January 1, 2025, they’re required by law to give every beneficiary standardized educational materials about generics. That means millions of seniors will get clear, accurate information directly from their drug plan.
What community health workers can do right now
You don’t need a medical degree to help patients understand generics. You just need the right tools.
- Use the FDA’s free Generic Drug Stakeholder Toolkit-it’s got printable handouts, conversation guides, and videos.
- Always explain: “Same medicine. Same dose. Same effect. Just cheaper.”
- Use the Teach-Back method: “Can you explain back to me why this pill is safe?”
- Address appearance changes head-on: “The color changed because the company that makes it is different. The medicine inside is exactly the same.”
- Share real numbers: “9 out of 10 prescriptions in the U.S. are generics. That’s millions of people using them safely every day.”
There’s no need to convince patients with jargon. Just give them facts in plain language. And then listen. Many patients just need to hear someone say, “I get why you’re worried. Let me show you why this is okay.”
What’s next for generic drugs
Over 287 brand-name drugs will lose patent protection between 2023 and 2028. That means more generics will hit the market. Some will be complex-like inhalers, eye drops, and creams. These are harder to copy. And that means patients might need more education.
The FDA already sees a 40% higher confusion rate with complex generics. That’s why they launched “Generics 101,” a video series for Medicare beneficiaries. Early results show a 31% boost in knowledge among viewers over 65.
What’s clear is this: the future of affordable healthcare depends on people trusting generics. Not because they’re cheap. But because they’re proven.
Final thought: It’s not about saving money. It’s about saving lives.
Generic drugs aren’t a compromise. They’re a solution. They let people with diabetes take their insulin. People with high blood pressure take their pills every day. People with depression stay on their medication because they can afford it.
Community health presentations aren’t just about handing out flyers. They’re about changing beliefs. One conversation at a time.


Barbara McClelland
November 29, 2025 AT 11:03I’ve seen this firsthand at the free clinic I volunteer at-patients will refuse a generic because it’s a different color, and then come back a week later saying they couldn’t afford their meds at all. We started using the FDA’s handouts and the ‘same medicine, same dose, same effect’ line, and wow-it changed everything. One lady told me, ‘I thought I was being cheated, but now I feel like I’m being helped.’ That’s the power of clear talk.
Alexander Levin
November 29, 2025 AT 17:48Ady Young
November 29, 2025 AT 21:18Man, I used to be one of those people who’d refuse generics until my dad got hit with a $400 insulin bill. We switched to the generic and he’s been stable for 3 years now. I didn’t realize how much fear was just based on looks-same pill, different packaging. The FDA’s data is rock solid. Why are we still fighting this?
Travis Freeman
December 1, 2025 AT 17:19This is so important. I work with refugees and a lot of them come from countries where fake meds are common, so they’re terrified of anything that looks ‘cheap.’ But when we sit down with them, show them the FDA stamp, and say, ‘This is what your doctor takes too’-they relax. It’s not about science alone. It’s about trust. And we can build that.
Sean Slevin
December 2, 2025 AT 15:10Chris Taylor
December 3, 2025 AT 12:03My grandma took her blood pressure med for 15 years-brand name. Switched to generic after Medicare changed her formulary. She didn’t notice a thing. Said the pills just looked ‘funny.’ We showed her the FDA page and she laughed. ‘So it’s just a new outfit?’ Yep. And now she saves $120 a month. She’s alive because of it.
Melissa Michaels
December 3, 2025 AT 19:58Nathan Brown
December 4, 2025 AT 00:02It’s funny how we trust a $500 brand-name pill more than a $12 generic-even though they’re chemically identical. We’ve been conditioned to equate price with quality. But what if the real quality is in the science, not the marketing? The FDA doesn’t care about logos. It cares about blood levels. And that’s the truth we need to keep repeating.
Matthew Stanford
December 4, 2025 AT 04:47My cousin in rural Kentucky couldn’t afford her asthma inhaler until she switched to the generic. She thought it wouldn’t work. We walked her through the FDA’s video on how inhalers are tested. Now she teaches other folks at the church group. It’s not about being smart-it’s about being heard. And sometimes, that’s all it takes.
Barbara McClelland
December 5, 2025 AT 15:42Just saw a comment about the nocebo effect-and you’re right. I had a patient who swore the generic made her dizzy. We swapped her back to the brand for a week, then back to generic-same pill, same dose. She said, ‘I didn’t even notice the difference this time.’ Turns out she was anxious about the switch, not the medicine. That’s the power of perception.