Capecitabine Dosing Calculator
Dosing Calculator
Dosing Result
Results will appear here after calculation
Standard dosing: 1000 mg/m² twice daily for 14 days in CAPOX regimen
Adjusted dose: mg/m² twice daily
Important: Always take within 30 minutes after a meal to improve absorption and minimize GI upset.
DPD Testing: Genetic testing recommended
Renal Adjustment:
Ever wondered how a pill can replace a drip for some cancer patients? Capecitabine started as a laboratory curiosity and now sits in the pocket of millions of oncology clinics worldwide. This article walks you through the science, the milestones, and the everyday realities of using this oral chemotherapy drug.
From Lab Bench to First Patient
In the early 1980s, researchers at the Royal Greenwich Hospital in London were hunting for a way to deliver fluorouracil (5‑FU) more selectively to tumors. Capecitabine is a fluoropyrimidine carbamate designed as a prodrug that becomes 5‑FU once inside the body. The key idea was to exploit enzymes that are over‑expressed in cancer tissue, letting the drug activate where it’s needed most.
By 1992, pre‑clinical studies in mice showed that the compound generated higher concentrations of 5‑FU within tumors than in normal tissue, paving the way for human trials. The first Phase I trial in 1995 confirmed that oral dosing could achieve therapeutic plasma levels without overwhelming toxicity.
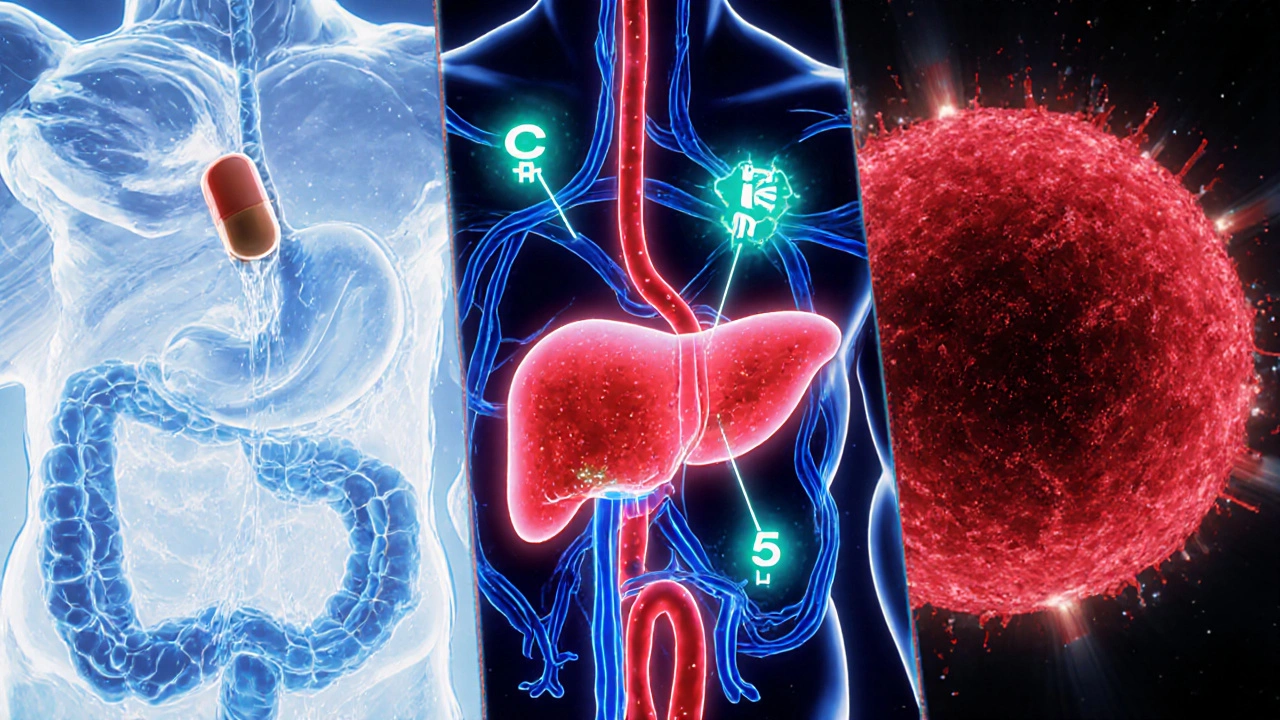
How Capecitabine Works Inside the Body
The drug’s journey begins when you swallow a tablet. It travels through the bloodstream to the liver, where the enzyme carboxylesterase removes a protective group, turning capecitabine into 5'-deoxy-5-fluorocytidine (5'-DFCR). Next, the enzyme cytidine deaminase converts 5'-DFCR to 5'-deoxy-5-fluorouridine (5'-DFUR). The final transformation happens inside the tumor itself, where Thymidine phosphorylase an enzyme highly expressed in many solid tumors cleaves 5'-DFUR to release the active chemotherapeutic Fluorouracil. Because thymidine phosphorylase is scarce in most normal tissues, the drug concentrates its effect where the cancer lives.
Once formed, 5‑FU interferes with DNA synthesis by inhibiting thymidylate synthase and incorporating into RNA, ultimately triggering cell death in rapidly dividing cells.
Regulatory Milestones and Global Approvals
The breakthrough data caught the eye of the U.S. Food and Drug Administration (FDA). In 1998, the FDA granted accelerated approval for capecitabine under the brand name Xeloda for metastatic colorectal cancer (mCRC) that had progressed after standard chemotherapy. Europe followed suit in 1999, and by the early 2000s the drug had expanded to breast and gastric cancer indications.
Key Phase III trials, such as the ECOG 4599 study for non‑small‑cell lung cancer and the B-31/NRG Oncology trial for HER2‑positive breast cancer, solidified capecitabine’s role as a backbone for combination regimens.
Current Indications: Who Gets Capecitabine Today?
- Metastatic colorectal cancer: Often used alone or combined with oxaliplatin (CAPOX regimen).
- Early‑stage breast cancer: Administered after surgery in combination with trastuzumab for HER2‑positive disease.
- Gastric and esophageal adenocarcinoma: Typically paired with cisplatin.
- Pancreatic cancer: Used in combination with gemcitabine for patients who cannot tolerate aggressive IV therapy.
Because the pill is taken at home, patients avoid the time‑consuming IV infusions that were once the only way to deliver 5‑FU.
Dosage, Scheduling, and Practical Tips
Standard dosing for the CAPOX regimen is 1,000 mg/m² of capecitabine taken twice daily for the first 14 days of a 21‑day cycle, alongside a 130 mg/m² IV infusion of oxaliplatin on day 1. For monotherapy in mCRC, the dose drops to 1,250 mg/m² twice daily on the same 14‑day schedule.
Therapeutic drug monitoring isn’t routine, but clinicians adjust doses based on renal function, age, and side‑effect profiles. A common rule of thumb: reduce the dose by 25% if the glomerular filtration rate (GFR) falls below 50mL/min.
Patients should take the drug within 30 minutes after a meal to improve absorption and minimize gastrointestinal upset.
Managing the Most Common Toxicities
While capecitabine spares many patients the inconvenience of an IV line, it brings its own set of side effects. The most frequently reported are:
- Hand‑foot syndrome a painful redness and swelling of the palms and soles.
- Diarrhea, often mild to moderate.
- Fatigue and nausea.
- Thrombocytopenia and neutropenia (less common than with IV 5‑FU).
Early detection is key. Patients are advised to keep skin moisturized, avoid heat, and report any tingling or blistering promptly. Dose reductions of 25% to 50% are standard when grade2 or higher hand‑foot syndrome develops.
Another crucial consideration is a genetic deficiency in Dihydropyrimidine dehydrogenase the enzyme that breaks down 5‑FU (DPD). Those with severe DPD deficiency can experience life‑threatening toxicity even at standard doses. Many centers now screen for DPYD gene variants before starting therapy.
Capecitabine vs. Intravenous 5‑FU: A Quick Comparison
| Aspect | Capecitabine (oral) | 5‑FU (IV) |
|---|---|---|
| Administration | Twice‑daily oral tablets | Continuous or bolus IV infusion |
| Convenience | Home‑based, no infusion center | Requires clinic visits |
| Targeted activation | Tumor‑specific via thymidine phosphorylase | Systemic activation |
| Common toxicity | Hand‑foot syndrome, diarrhea | Cardiotoxicity, severe mucositis |
| Cost (US 2025) | ~$2,800 per 3‑month cycle | ~$3,500 per 3‑month cycle (including infusion supplies) |
Both agents ultimately deliver 5‑FU, but the oral route offers quality‑of‑life benefits for many patients, especially those living far from oncology centers.

Future Directions: Combining Capecitabine with New Technologies
Research is now looking at pairing capecitabine with immune checkpoint inhibitors. Early‑phase trials suggest that the immunogenic cell death caused by 5‑FU can synergize with PD‑1 blockade, potentially widening the drug’s effect beyond traditional indications.
Another promising avenue is nanocarrier delivery. By encapsulating capecitabine in liposomal particles, scientists aim to further increase tumor selectivity and reduce hand‑foot syndrome rates.
Finally, pharmacogenomic testing for DPYD variants is becoming a standard pre‑treatment step in many European hospitals, ushering in a new era of personalized dosing that could make capecitabine safer for a broader patient pool.
Quick Takeaways
- Capecitabine is an oral prodrug that converts to 5‑FU preferentially inside tumor cells.
- Approved first for metastatic colorectal cancer in 1998, now used in breast, gastric, pancreatic, and other solid tumors.
- Key enzymes: carboxylesterase, cytidine deaminase, and thymidine phosphorylase.
- Common side effects include hand‑foot syndrome and diarrhea; DPD deficiency screening is essential.
- Oral administration offers convenience and comparable efficacy to IV 5‑FU, with a distinct toxicity profile.
Frequently Asked Questions
What types of cancer can be treated with capecitabine?
Capecitabine is approved for metastatic colorectal cancer, early‑stage HER2‑positive breast cancer (often with trastuzumab), gastric and gastro‑esophageal junction adenocarcinoma, and as part of combination regimens for pancreatic cancer. Off‑label use also includes certain head‑and‑neck cancers.
How does capecitabine differ from intravenous 5‑FU?
Both deliver the same active molecule, 5‑FU, but capecitabine is taken orally and relies on tumor‑specific enzymes for activation, which can reduce systemic side effects. IV 5‑FU is given directly into the bloodstream, requiring clinic visits and often causing different toxicities like cardiotoxicity.
What is hand‑foot syndrome and how can I prevent it?
Hand‑foot syndrome is redness, swelling, and sometimes blistering on the palms and soles caused by capecitabine. Preventive measures include keeping the skin moisturized, avoiding hot water, tight shoes, and manual labor. If symptoms appear, report them early so your doctor can adjust the dose.
Should I get genetic testing before starting capecitabine?
Yes, testing for DPYD gene variants that affect dihydropyrimidine dehydrogenase activity is recommended. Patients with reduced DPD function are at high risk for severe toxicity and often need a dose reduction or an alternative therapy.
Can capecitabine be taken with food?
The drug should be taken within 30 minutes after a meal. Food increases absorption and reduces stomach irritation, making the regimen easier to tolerate.

genevieve gaudet
October 17, 2025 AT 21:40Ever think about how a pill can become a tiny lab inside your body? Capecitabine kinda proves that modern medecine is more alchemy than black‑box, turning a simple tablet into a targeted killer of cancer cells. It's like the universe gave us a clever shortcut, and we just had to figure out the right spell. Still, we gotta ask ourselves if convenience ever truly beats the raw, hands‑on approach.
Patricia Echegaray
October 18, 2025 AT 03:13Look, the pharma elites pushed capecitabine as some miracle cure while they sit on piles of cash, and the media just gushes over the “convenience” like it’s a patriotic duty. They’re selling us a pill‑promoted illusion, hoping we forget the hidden costs and the secret trials they hide behind FDA red tape. It’s a classic case of corporate overlords manipulating the health system for their own gain, and we’re supposed to cheer because it’s “American innovation.” 🚩
Cindy Thomas
October 18, 2025 AT 08:46Actually, the data behind capecitabine is solid-randomized trials show it matches IV 5‑FU in many settings, and the convenience factor saves patients countless hospital trips 😊. While some love a good conspiracy, the real story is about rigorous science and patient‑centered care, not hidden agendas.
Kate Marr
October 18, 2025 AT 17:06Nothing beats a home‑grown solution that lets our brave patients fight cancer without endless trips to the hospital 🇺🇸💪. Capecitabine gives us the freedom to keep fighting from our own kitchens and living rooms, a true testament to American ingenuity 😎.
James Falcone
October 19, 2025 AT 01:26America deserves the best cancer care, period.
Frank Diaz
October 19, 2025 AT 07:00Such bravado overlooks the nuanced ethics of drug distribution; glorifying a medication without acknowledging its side‑effects reduces patients to mere statistics in a nationalistic march. True wisdom demands we balance pride with humility.
Mary Davies
October 19, 2025 AT 15:20Isn't it fascinating how a simple capsule can hold the weight of hope and terror alike? The narrative of capecitabine reads like a drama-science scribbles a script, doctors deliver the act, and patients sit in the front row, breath held. Yet, behind the curtain, there are stories of trials, setbacks, and silent battles that rarely make the headlines.
Valerie Vanderghote
October 19, 2025 AT 20:53The journey of capecitabine from a bench top curiosity to a household name in oncology is nothing short of a modern epic.
It began in the humid labs of Greenwich, where scientists first whispered about a prodrug that could sneak past normal tissues.
Over the next decade, mice were dosed, data were plotted, and doubts were whispered in conference halls.
When the first human trials emerged, the world watched a modest pill challenge the towering IV drips of the past.
The mechanism, reliant on tumor‑specific enzymes, felt like a secret handshake between chemistry and biology.
Patients, once chained to infusion chairs, suddenly found themselves reaching for a bottle of tablets rather than a needle.
Yet this freedom brought its own demons, as hand‑foot syndrome painted a painful picture on palms and soles.
Clinicians learned to temper doses, to moisturize skin, and to warn of the fiery tingles that could precede blisters.
Genetic testing for DPD deficiency added another layer of personalization, sparing the vulnerable from fatal toxicity.
Meanwhile, health economists crunched numbers, debating whether the oral route truly saved money or simply shifted costs.
The drug’s entry into breast, gastric, and pancreatic regimens illustrated the adaptability of a once‑narrow indication.
Research now peers into the future, coupling capecitabine with checkpoint inhibitors in hopes of a synergistic spark.
Nanocarriers whisper promises of even tighter tumor targeting, perhaps finally quieting the hand‑foot torment.
Across continents, patients share stories on forums, swapping tips on managing side effects and celebrating small victories.
In the grand tapestry of cancer therapy, capecitabine stands as a reminder that innovation often arrives disguised as a humble pill, reshaping lives one dose at a time.
Michael Dalrymple
October 20, 2025 AT 10:46From a therapeutic standpoint, capecitabine exemplifies the principle of targeted prodrug activation, aligning pharmacologic precision with patient quality of life. As clinicians, we bear the responsibility to educate patients on dosing schedules, monitor renal function, and pre‑emptively address toxicities such as hand‑foot syndrome. Incorporating DPYD genotyping into the treatment algorithm reflects our commitment to personalized medicine, reducing the risk of severe adverse events. Moreover, the oral administration paradigm empowers patients, fostering adherence and reducing the logistical burdens associated with infusion centers. Ultimately, the drug’s evolution underscores the collaborative nature of oncology, where research, regulation, and compassionate care converge to improve outcomes.
Emily (Emma) Majerus
October 20, 2025 AT 16:20Great rundown-just remember to keep the meds with food, it helps absorption 👍.
Virginia Dominguez Gonzales
October 20, 2025 AT 21:53What a journey we’ve witnessed! From lab benches to living rooms, capecitabine has transformed the battle against cancer, and every patient’s triumph adds a brilliant stanza to this ongoing saga. Let’s continue to champion education, empathy, and vigilant care as we walk beside those who brave this fight.
Alexis Howard
October 21, 2025 AT 03:26Sure the data looks good but why trust the hype it feels like marketing fluff