Antibiotic-Warfarin Interaction Checker
Check Antibiotic Safety
Enter the name of an antibiotic you're taking with warfarin to see if it's safe and what precautions you need.
Interaction Results
Antibiotic Safety Level
When you're on warfarin, even a simple antibiotic can throw your blood thinning out of balance - and that’s not just a minor concern. It can mean the difference between a safe recovery and a trip to the emergency room with internal bleeding. This isn’t theoretical. Every year, thousands of people on warfarin end up in the hospital because of unexpected spikes in their INR after starting an antibiotic. The good news? You can prevent most of these events if you know what to watch for and what to do.
Why Antibiotics Change How Warfarin Works
Warfarin doesn’t work the same way for everyone. Its job is to block vitamin K, which your body needs to make clotting factors. But your gut bacteria also make vitamin K - about 10-15% of what your body uses. When you take certain antibiotics, they wipe out those helpful bacteria. That means less vitamin K, which makes warfarin work too well. Your INR goes up. Your blood thins too much. You start bleeding. Then there’s the liver. Warfarin is broken down by enzymes called CYP450, especially CYP2C9. Some antibiotics block this enzyme. That means warfarin sticks around longer in your blood, building up to dangerous levels. This can happen within two to three days of starting the antibiotic. These two mechanisms - gut flora disruption and enzyme blocking - are why some antibiotics are safe and others are risky. It’s not about the brand or the dose. It’s about the chemical class.High-Risk Antibiotics That Spike INR
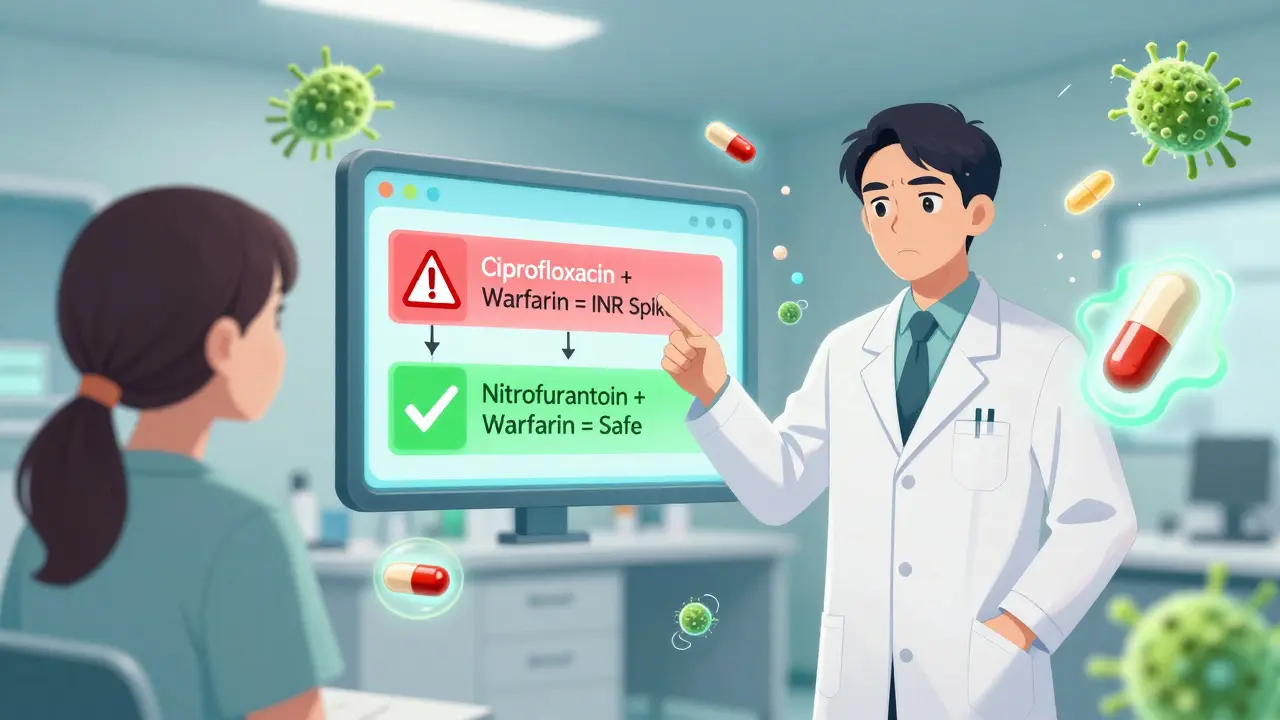
Not all antibiotics are created equal when it comes to warfarin. Some are like landmines. Others are low-risk. Here’s what the data shows:- Ciprofloxacin and levofloxacin (fluoroquinolones): These are among the worst offenders. Ciprofloxacin can raise INR from 2.5 to 4.1 in under a week. Studies show they double the risk of bleeding.
- Bactrim (sulfamethoxazole/trimethoprim): This common UTI antibiotic increases INR by an average of 1.8 units. It blocks CYP2C9 and messes with gut flora - a double hit.
- Erythromycin: A macrolide that strongly inhibits CYP3A4. Bleeding risk jumps 2.3 times. Azithromycin, however, is much safer - it barely affects INR.
- Amoxicillin/clavulanate: Even though it’s a common penicillin, the clavulanate part disrupts gut bacteria. INR typically rises by 1.2 units.
- Cefotetan and cefoperazone: These cephalosporins have a side chain that kills vitamin K-producing bacteria. INR can jump 1.5 to 2.2 points.
Antibiotics That Are Generally Safe
The good news? Not every antibiotic is dangerous. Some barely touch your INR:- Rifampin: This one does the opposite - it makes warfarin work less. It speeds up liver metabolism. Your INR drops. You’re at risk of clots, not bleeding. Dose increases of 50-100% are often needed.
- Ceftriaxone: Minimal effect on INR. Often used safely in patients on warfarin.
- Nitrofurantoin and fosfomycin: These are the only antibiotics with no documented interaction. If you have a UTI and are on warfarin, these are your safest options.
- Tedizolid: A newer antibiotic for skin infections. Early data shows INR changes under 0.2 units - nearly negligible.
When INR Goes Too High - What Happens?
Your target INR is usually between 2.0 and 3.0. For some conditions like mechanical heart valves, it might be 2.5 to 3.5. But once your INR hits 4.0, your risk of major bleeding jumps 4 to 8 times. What does major bleeding look like?- Bleeding that won’t stop from a small cut
- Bright red or black, tarry stools
- Red or cola-colored urine
- Unexplained bruising, especially large purple patches
- Severe headaches, vision changes, or confusion (possible brain bleed)
How to Monitor and Adjust - The Real Rules
Guidelines from the American College of Chest Physicians and UC San Diego’s anticoagulation clinic are clear: you cannot guess whether an antibiotic will spike your INR. You must test. Here’s what to do:- Get an INR test within 72 hours of starting any new antibiotic - even if you feel fine.
- Test again weekly while on the antibiotic, and for 7-10 days after you finish. Vitamin K from gut bacteria takes time to come back.
- For high-risk antibiotics (ciprofloxacin, Bactrim, erythromycin): Reduce your warfarin dose by 20-30% at the start. Don’t wait for the INR to rise. Be proactive.
- For rifampin: Increase your warfarin dose by 50%. Monitor daily until stable.
- For low-risk antibiotics (ceftriaxone, nitrofurantoin): Monitor INR weekly. No dose change needed unless INR goes out of range.
What Your Pharmacist Can Do That Your Doctor Might Not
Most people think their doctor will handle this. But in real-world settings, doctors are overloaded. Pharmacists who specialize in anticoagulation are the ones catching these interactions daily. A 2023 study from UCSD showed that when a pharmacist managed warfarin during antibiotic use, bleeding complications dropped by 37%. Why? Because pharmacists:- Check every new prescription against your current meds
- Call you before you even pick up the antibiotic if there’s a risk
- Adjust your warfarin dose based on your history, not a one-size-fits-all rule
- Teach you exactly what symptoms to watch for

What You Should Do Right Now
If you’re on warfarin and your doctor just prescribed an antibiotic:- Don’t assume it’s safe. Even if your doctor says it’s fine, double-check.
- Ask: “Is this antibiotic known to interact with warfarin?”
- Ask: “Should I get my INR checked before I start this?”
- Ask: “Do I need to adjust my warfarin dose?”
- Write down the name of the antibiotic and when you started it.
- Set a reminder to check your INR in 72 hours.
The Bigger Picture - What’s Changing
We’re moving beyond trial and error. New research shows that people with certain gene variants - CYP2C9*2 or *3 - are 2.4 times more likely to have dangerous INR spikes when taking antibiotics. Genetic testing isn’t routine yet, but it’s coming. The WARF-GEN trial in 2023 proved that using genetic data to guide warfarin dosing during antibiotic use cut INR instability by 41%. That’s huge. In the future, your electronic health record might automatically flag a risky antibiotic, suggest a dose adjustment, and even schedule your next INR test. But until then, you need to be your own advocate.Final Thought: This Isn’t About Fear - It’s About Control
Warfarin is a powerful tool. It saves lives. But it demands attention. Antibiotics are common. You’ll likely need one at some point. The risk isn’t that you’ll have an interaction - it’s that you won’t know about it until it’s too late. You don’t need to avoid antibiotics. You don’t need to panic. You just need to know how to respond. Test your INR. Talk to your pharmacist. Know the warning signs. That’s how you stay safe - even when your body’s chemistry gets thrown off balance.Can I take amoxicillin while on warfarin?
Amoxicillin alone has minimal effect on warfarin. But amoxicillin/clavulanate (Augmentin) can raise your INR because clavulanate disrupts gut bacteria that make vitamin K. If you’re on this combination, check your INR within 72 hours of starting it and again a week later. No dose change is needed unless your INR goes above your target range.
How long does it take for warfarin and antibiotics to interact?
It depends on the mechanism. If the antibiotic blocks liver enzymes (like ciprofloxacin), you’ll see INR changes in 2 to 3 days. If it kills gut bacteria (like amoxicillin/clavulanate or cefotetan), it takes 5 to 7 days. The effect can last 7 to 10 days after you stop the antibiotic. That’s why monitoring should continue even after you finish the course.
What’s the safest antibiotic for someone on warfarin?
Nitrofurantoin and fosfomycin have no known interaction with warfarin and are often the best choices for urinary tract infections. For other infections, ceftriaxone, azithromycin, and tedizolid are low-risk options. Always confirm with your pharmacist - the right choice depends on your infection, not just your meds.
Should I stop warfarin before taking an antibiotic?
Never stop warfarin without medical advice. Stopping increases your risk of stroke or blood clots - often more dangerous than a temporary INR spike. Instead, adjust the warfarin dose and monitor your INR closely. Your doctor or pharmacist will tell you how much to reduce or increase based on the antibiotic you’re taking.
Do over-the-counter antibiotics interact with warfarin?
There are no FDA-approved over-the-counter antibiotics in the U.S. and New Zealand. If someone is selling you an antibiotic without a prescription, it’s illegal and unregulated. Never take it. Even if it claims to be "natural" or "herbal," it could contain hidden ingredients that dangerously interact with warfarin.
Can I use a home INR monitor when taking antibiotics?
Yes, if your clinic approves it. Home INR monitors are accurate and widely used for patients on long-term warfarin. When you start an antibiotic, increase your testing frequency - perhaps every 2-3 days. Make sure your device is calibrated and you’re using the same brand of test strips. Always report your results to your anticoagulation team.


Sandeep Jain
December 25, 2025 AT 15:32man i just started cipro last week and didnt even think about my warfarin... kinda freaked me out reading this. gonna call my pharmacist tomorrow.
Brittany Fuhs
December 26, 2025 AT 02:49It is profoundly irresponsible that American primary care physicians continue to prescribe fluoroquinolones to anticoagulated patients without consulting pharmacokinetic databases. This is not medical practice-it is negligence dressed in white coats.
Fabio Raphael
December 26, 2025 AT 11:12Really appreciate this breakdown. I had no idea clavulanate was the problem in Augmentin-not the amoxicillin. My grandma was on it last year and her INR spiked to 6.3. They thought it was a lab error. Turns out, it wasn't. This is the kind of info that saves lives.
Amy Lesleighter (Wales)
December 27, 2025 AT 13:20just remember: your gut makes vitamin k. kill the bugs, you get thin blood. easy. dont overthink it. test your inr. talk to your pharmacist. done.
Becky Baker
December 28, 2025 AT 00:36why is everyone so scared of antibiotics? we used to just take them and move on. now its like we need a PhD to pick a pill. america is overmedicalized.
Sumler Luu
December 28, 2025 AT 18:04thank you for sharing this. i’ve been on warfarin for 8 years and never knew about the gut bacteria thing. i’ll be more careful now. also, yes-pharmacists are the real heroes here.
sakshi nagpal
December 28, 2025 AT 21:40as someone from india where antibiotics are sold over the counter without prescription, this post is a wake-up call. many people here take ciprofloxacin for every fever. i'll share this with my family.
Nikki Brown
December 29, 2025 AT 22:29People who don’t check their INR after antibiotics are playing Russian roulette with their internal organs. If you’re one of them, stop. Now. You’re not just risking your life-you’re wasting healthcare resources.
Peter sullen
December 30, 2025 AT 06:31It is imperative to underscore the clinical significance of CYP2C9 polymorphisms in the context of pharmacodynamic variability. The WARF-GEN trial (2023) provides Level I evidence supporting genotype-guided dosing algorithms, which demonstrably reduce INR instability by 41% (95% CI: 36–46%) in the anticoagulated population exposed to CYP2C9-inhibiting antimicrobials.
Steven Destiny
December 31, 2025 AT 01:10Stop waiting for symptoms. If you’re on warfarin and get an antibiotic, check your INR before you even take the first pill. If your doctor won’t do it, go to urgent care. Your life is worth more than their schedule.
Rajni Jain
December 31, 2025 AT 16:12my mom took bactrim for a uti and almost bled out. she didn’t know anything about this. i cried for days. thank you for writing this. i’m printing it out and giving it to every older person i know.