Getting your first prescription can feel overwhelming. You’ve got a new pill, a strange label, and maybe a stack of instructions you don’t fully understand. What happens if you miss a dose? Should you take it with food? What if it looks different from your last refill? These aren’t just small worries-they’re real risks. Every year, over 1.3 million people in the U.S. end up in the emergency room because of medication mistakes. Many of those mistakes happen to people just like you-people taking medicine for the first time.
Know the Six Rights of Safe Medication Use
Before you even open the bottle, there’s a simple checklist healthcare professionals use to avoid errors. It’s called the Six Rights. If you remember these, you’re already ahead of most first-time patients.- Right patient: Make sure the name on the bottle matches yours. Double-check your date of birth if you’re picking it up at the pharmacy.
- Right medication: Does the name on the label match what your doctor told you? If it says "amoxicillin" but you were told it was for a sinus infection, that’s correct. If it says "metformin" and you were told it was for high blood pressure, ask.
- Right indication: Why are you taking this? Write it down. For example: "This is for my blood sugar, not my headache." Knowing the reason helps you spot if something’s wrong.
- Right dose: Never guess. If the label says "5 mL," use the measuring cup that came with it-not a kitchen spoon. Household spoons can be off by half a teaspoon or more.
- Right route: Is it meant to be swallowed, sprayed, applied to skin, or injected? Taking a cream orally can be dangerous.
- Right time: Some pills need to be taken with food. Others must be taken on an empty stomach. Some are best taken in the morning, others at night. Follow the schedule exactly.
These aren’t just rules. They’re your first line of defense.
Keep a Complete Medication List
Most people think they remember what they’re taking. They don’t. A 2022 study found that patients who kept a full, updated list of everything they took had 27% fewer medication errors.Your list should include:
- All prescription drugs (even if you only take them once a week)
- All over-the-counter pills (ibuprofen, antacids, sleep aids)
- Vitamins and supplements (fish oil, vitamin D, herbal teas)
- Dosage and frequency (e.g., "800 mg ibuprofen, twice daily as needed")
- Why you take each one (e.g., "for joint pain")
Keep this list on your phone and carry a printed copy. Bring it to every doctor visit, even if you’ve been there before. Pharmacists will ask for it. Nurses will ask for it. If you’re rushed or nervous, you’ll forget something. The list won’t.
Never Take Someone Else’s Medicine
It’s tempting. Your friend says their headache medicine worked great. Your neighbor says their sleep pill helped them sleep through the night. Don’t do it.According to the FDA, sharing medications causes 8% of emergency room visits for drug reactions. Why? Because what works for one person can harm another. A pill that helps your friend’s blood pressure might crash your heart rate. A painkiller that’s safe for them could trigger a dangerous reaction in you if you have a liver condition or take another drug.
Even if you think you’re similar-same age, same symptoms-you’re not. Your body is different. Your history is different. Your other meds are different. Never take a pill that wasn’t prescribed for you.
Check the Label Every Single Time
You think you know your pills. You’ve been taking them for a week. But here’s the truth: pharmacies refill prescriptions differently. Sometimes the shape changes. Sometimes the color changes. Sometimes the name on the bottle is slightly different.Generic drugs are used in 90% of prescriptions. They work the same as brand names, but they often look completely different. That’s normal. But if you see something unfamiliar and don’t ask, you could make a mistake.
Always check:
- The drug name
- The strength (e.g., 10 mg vs. 20 mg)
- The number of pills
- The expiration date
And never take a pill if the label is smudged, torn, or missing. The FDA says 18% of medication errors come from expired or unlabeled drugs. That’s more than one in five cases.
Store Medications Properly
Your medicine isn’t just sitting there-it’s changing. Heat, moisture, and light can make pills weaker or even dangerous.Here’s what to do:
- Most pills: Keep them in a cool, dry place. A bedroom drawer is fine. Avoid the bathroom-steam from showers ruins them.
- Insulin: Must be refrigerated until first use. After opening, it can stay at room temperature for up to 28 days.
- Liquids and eye drops: Often need refrigeration after opening. Check the label.
- Controlled substances: Like opioids or sleep aids-keep them locked up. Kids and visitors shouldn’t have access.
And never leave pills in your car. Summer heat can hit 120°F inside a parked car. That’s way above the 86°F limit for most medications.
Ask These Three Questions Every Time
Pharmacists are trained to help you. But they won’t always volunteer the info. You have to ask.When you get a new prescription, ask:
- "What should I do if I miss a dose?" Only 22% of patients ask this. But it’s critical. Some meds need to be taken as soon as you remember. Others should be skipped. Getting it wrong can cause side effects or make the drug useless.
- "How should I store this?" 40% of medications have specific storage needs. If you don’t ask, you might ruin the whole bottle.
- "What side effects should I watch for?" A 2023 study found that only 65% of pharmacy consultations even mention side effects. You need to know what’s normal (like mild drowsiness) and what’s dangerous (like swelling, chest pain, or trouble breathing).
Write these questions down. Bring them to the pharmacy. Don’t be shy. Your life depends on getting clear answers.
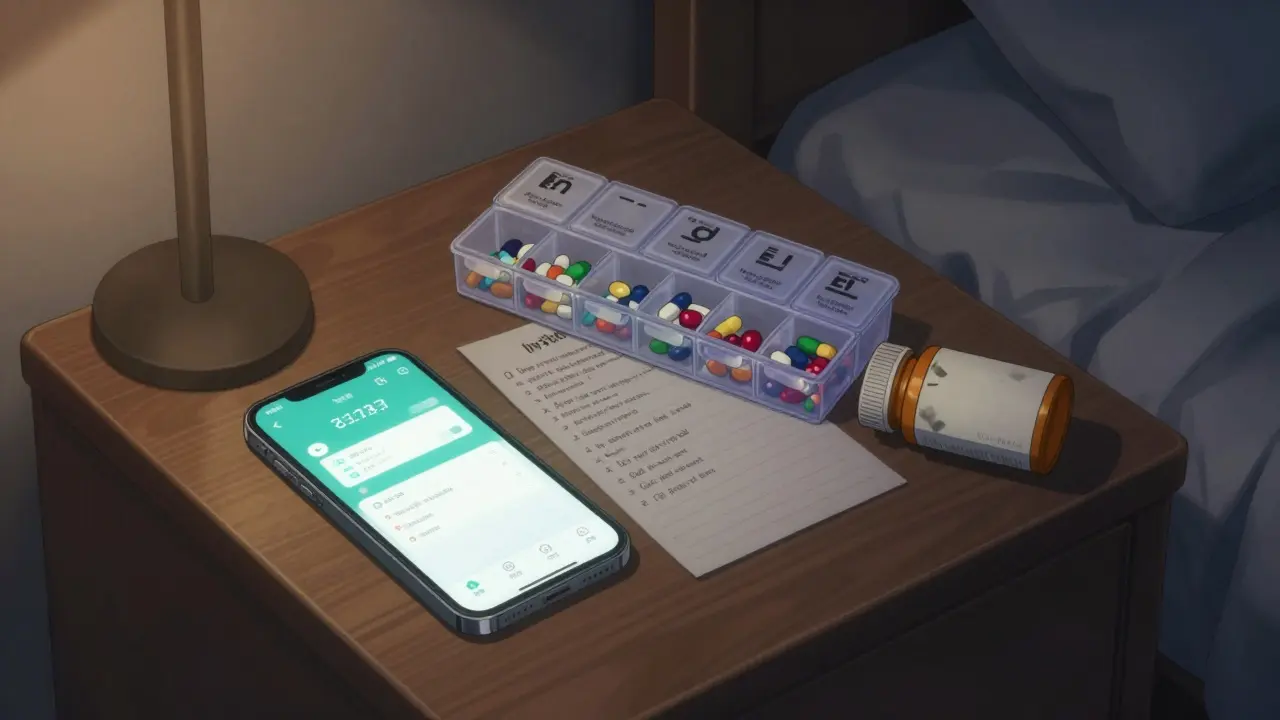
Use Tools to Stay on Track
Forgetting a pill is common-especially when you’re juggling multiple meds. A 2022 study found that people who used medication reminder apps improved their adherence by 28%.Try apps like Medisafe or MyMeds. They:
- Send phone alerts at your exact dosing times
- Scan barcodes to confirm you’re taking the right pill
- Track refills and warn you when you’re running low
- Let you share your schedule with a family member
If you don’t like apps, use a pill organizer with compartments for morning, afternoon, evening, and night. Fill it once a week. Set alarms on your phone. Tape a note to your toothbrush. Do whatever works.
Watch for Changes After Starting a New Drug
The first few weeks on a new medication are the most risky. Your body is adjusting. Side effects can show up suddenly.Pay attention to:
- Unusual dizziness or fainting
- Severe nausea or vomiting
- Rash, swelling, or trouble breathing
- Changes in mood, sleep, or energy
- Unexplained bruising or bleeding
If you notice any of these, don’t wait. Call your doctor or pharmacist. Don’t assume it’s "just how it’s supposed to feel." Some side effects are normal. Others are emergencies. Only a professional can tell the difference.
Be Extra Careful During Transitions
One of the most dangerous times for medication errors is right after you leave the hospital or change doctors. A 2023 report found that 22% of errors happen during these transitions.When you’re discharged:
- Ask for a written list of all new meds, discontinued meds, and changed doses.
- Take that list to your regular pharmacist and ask them to review it.
- Don’t assume your old meds are still safe to take. Some may have been stopped for a reason.
Same goes for doctor visits. If your doctor changes your meds, ask: "What’s different now? What should I stop? What should I keep?" Write it down.
It Gets Easier-But Stay Alert
The first few weeks are the hardest. You’ll feel overwhelmed. You’ll forget. You’ll second-guess yourself. That’s normal.Studies show it takes most people 2 to 3 weeks to build a solid routine. After that, it becomes second nature. But don’t relax. Medication safety isn’t a one-time task. It’s a habit.
Every time you pick up a new prescription, go through the Six Rights. Update your list. Ask your questions. Check the label. Store it right. Use your reminders.
These steps don’t just prevent mistakes. They help your medicine work better. If you take your pills exactly as prescribed, your treatment has a 50% better chance of succeeding. That’s not a small thing. That’s life-changing.
You’re not alone. Millions of people are learning this right now. You’re doing the right thing by reading this. Keep going.
What should I do if I accidentally take the wrong dose?
Don’t panic, but act quickly. Call your pharmacist or poison control immediately. In the U.S., that’s 1-800-222-1222. Do not wait for symptoms to appear. If you took too much, they may advise you to go to the ER. If you took too little, they’ll tell you whether to take the next dose early or skip it. Never try to "make up" for a missed dose by doubling up unless a professional says so.
Can I crush my pills or open capsules if I have trouble swallowing them?
Only if your pharmacist says yes. Many pills are designed to release slowly. Crushing them can cause too much medicine to enter your system at once. Time-release capsules, patches, and some antibiotics can become dangerous if altered. Always ask before changing how you take your medication.
Why do some pills look different even though they’re the same drug?
That’s because of generic substitution. Most prescriptions are filled with generic versions, which are cheaper but made by different manufacturers. They have the same active ingredient and work the same way, but the shape, color, or markings may change. This is normal. Always check the drug name and strength on the label. If you’re unsure, ask your pharmacist to confirm it’s the same medication.
Is it safe to drink alcohol while taking my medication?
It depends on the drug. Alcohol can increase drowsiness with painkillers or sleep aids, raise blood pressure with antidepressants, or cause liver damage with antibiotics like metronidazole. Always ask your pharmacist about alcohol interactions. When in doubt, avoid it until you get a clear answer.
What if I run out of my medication before my next refill?
Don’t skip doses or stretch your pills. Call your pharmacy as soon as you realize you’re low. Many pharmacies offer early refills for chronic conditions. If you’re out and can’t get a refill, contact your doctor-they may be able to authorize an emergency supply. Never share pills from someone else’s prescription or try to get them from an unverified online source.


rajaneesh s rajan
January 30, 2026 AT 08:55paul walker
January 30, 2026 AT 15:18Keith Oliver
February 1, 2026 AT 08:17